Earlier this month, an article was featured in The New York Times again highlighting the ongoing issues related to death of women in the U.S. during their pregnancy or in the delivery of their babies. This comes months after the USA Today article that originally brought attention to maternal mortality rate. These articles describe the national maternal mortality crisis, highlighting the alarming fact that the U.S. has the highest maternal death rate among the world’s developed nations. A rate that has continued to rise, while the death rate has been stable or falling in other developed countries.
The main differences between the two articles is the progression of time from one to the other that allowed for additional sources of concern, such as the high rate of cesarean delivery in low-risk, first-time pregnant women and including the risks associated with unwarranted surgeries playing into the national maternal mortality rate. Obstetrical hemorrhage, unmanaged and uncontrolled hypertensive disorders in pregnancy, and high rates of cesarean deliveries on low-risk mothers all introduce risk to an already vulnerable population.
The Response to Reduce Maternal Mortality
To address the maternal mortality national crisis, the U.S. Government has just recently responded by creating the Preventing Maternal Deaths Act that was signed in December of 2018. This Act provides for federal dollars to fund maternal mortality review committees for states that currently do not have one. These committees are charged with reporting their review findings, and then developing recommendations and information on interventions to the Director of the CDC.
This approach has proven to be effective in understanding what went wrong in these cases of mothers dying during pregnancy or for up to one year following their delivery. It’s incredibly important work and many would say it’s long overdue. But at least it’s happening and for that we can be thankful.
Additionally, Congress has reached out to the largest health systems in the country (accounting for the majority of births in the U.S.), to understand how maternal mortality has historically been managed. The inquiry is quite extensive but specifically targeted to uncover what these largest healthcare delivery systems have done and are doing to be identify, be aware of, and manage disparities in care, variation in care delivery patterns and what protocols they’re using and how they’re managing deviation from the national evidence-based guidelines.
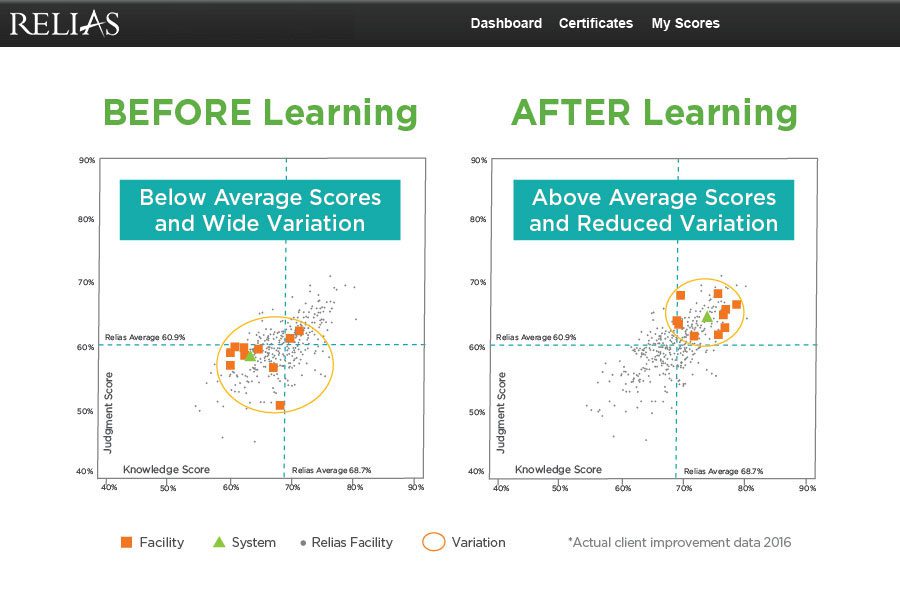
Every pregnant woman should receive equal evidence-based care no matter their socioeconomic and race/ethnicity factors. The reality is – there is significant amounts of variation in care despite the national evidence-based guidelines and protocols focused on care in the areas where women die most commonly in pregnancy and after delivery.
As part of the inquiry they want to know:
- How are they identifying and managing disparities in maternal care, health risk and health outcomes?
- What education, if any, are health care delivery clinicians (physicians and nurses) receiving and does it make a difference in competency and delivering safe effective care to everyone regardless of social or ethnic background?
Again – in the hospital, death and harm to a mother is largely attributed to hypertensive disorders in pregnancy and obstetrical hemorrhage and unnecessary cesarean births. This high level of clinical practice variation from hospital to hospital, from provider to provider, from care team to care team, is not only unnecessary, it comes with a cost of compromising patient safety.
Addressing this variation and ultimately, variation in care delivery patterns, is of the utmost importance as we work to improve patient safety and develop a culture of high reliability for one of our nation’s most vulnerable patient populations – our mothers and their babies.
A Timely Relias Resource
In this Promoting Vaginal Birth: A Guide to Understand and Lower the Cesarean Birth Rate whitepaper, Relias clinical experts discuss the unacceptably high rate of cesarean births along with the associated short and long-term risks to both mothers and babies when these procedures are not medically necessary.
Access the whitepaper to learn:
- Four contributors to higher cesarean birth rates
- Strategies to promote physiologic birth and the importance of patient education
- The role of induction: recent trends, appropriate use, and associated risks
- The use of FHR management guidelines
- Increasing access to vaginal birth including management of singleton breech, twins, and TOLAC
How Relias Can Help
For more than 20 years, Relias has helped hospitals identify and reduce variation in care and improve patient safety with analytics, provider and nurse assessments, and evidence-based education tailored to the individual. Relias OB, formerly GNOSIS™ OB, offers a suite of AWHONN validated and co-authored courses for providers and nurses on Promoting Vaginal Birth, Fetal Assessment and Monitoring, Shoulder Dystocia, Obstetrical Hemorrhage, and Hypertensive Disorders in Pregnancy.
Relias OB
Reducing variation in care delivery saves lives, but if you don’t measure variation, how do you know?
Learn More →





