Heroin is an opiate drug that is synthesized from morphine, a naturally occurring substance extracted from the seed pod of the Asian opium poppy plant. It usually appears as a white or brown powder or as a black sticky substance, known as “black tar heroin.” It can be injected, inhaled by snorting, sniffing, or smoked.
Facts and Figures
Per a July 2015 report by the U.S. Centers for Disease Control and Prevention (CDC):
- Heroin use more than doubled among young adults ages 18–25 in the past decade
- The heroin-related overdose death rate increased 286% from 2002 to 2013
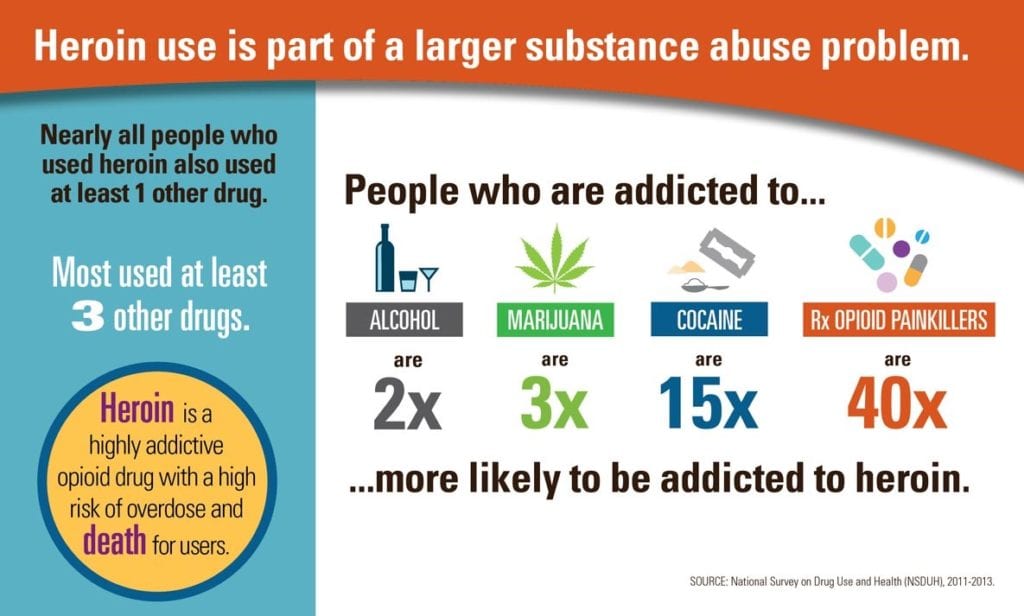
- More than 9 in 10 people who used heroin also used at least one other drug
Officials say the skyrocketing trend is partly fueled by increased numbers of persons addicted to prescription pain medications. Per the CDC, among new heroin users during 2000 to 2013, approximately three out of four report having misused prescription opioids prior to using heroin.
Those addicted to prescription opioid pain medications are 40 times more likely to become addicted to heroin. People addicted to prescription pain medications often switch to heroin because it offers a similar high, doesn’t require a prescription, and is cheaper to buy.
High Risk for Addiction & Health Risks
All routes of administration deliver the drug to the brain very rapidly, which contributes to the high risk for addiction and health risks. Opiate abusers develop a tolerance, or the need to use larger amounts to achieve the same effects. Addiction occurs when a person requires regular and increasing doses to function normally in daily life. Changes in the brain from use of the drug are known to cause uncontrollable drug-seeking behaviors, no matter the consequences.
Users of heroin report feeling a rapid surge of euphoria followed by a pleasant drowsiness. This is accompanied by dry mouth, a warm flushing of the skin, heaviness of the extremities, and clouded mental functioning. Initial highs last from 4 to 6 hours, but once tolerance is developed, highs are reduced to 2 to 4 hours.
When heroin enters the brain, it is converted back into morphine, which binds to molecules on cells known as opioid receptors that control perception of pain and reward. These receptors also control processes critical for life, such as blood pressure, arousal, and respiration. Heroin overdoses frequently involve a suppression of breathing, which reduces the amount of oxygen that reaches the brain. This can have short- and long-term psychological and neurological effects, including coma, permanent brain damage, and death.
Signs, Symptoms, and Effects of Heroin Abuse
The signs and symptoms of heroin addiction vary among users, but the most common include:
- Depression
- Euphoria
- Dry mouth
- Warm, flushed skin
- Constricted pupils
- “Nodding off” during conversations
- Shortness of breath
- Extreme itching
- Anxiety, hostility, agitation, and irritability
- Disorientation
- Hallucinations
- Paranoia and delusions
- Track marks on arms and legs
- Scabs or bruises as a result of picking at the skin
- Weight loss
- Decreased attention to personal hygiene
- Possession of burned spoons, needles or syringes, missing shoelaces, glass pipes
- Periods of hyperactivity followed by periods of exhaustion and sleeping
- Apathy, lack of motivation, decline in occupational or academic performance
The effects of heroin abuse differ depending on the length of abuse, amount of heroin used, presence of other substances, and individual health factors. The severity of symptoms tends to worsen the longer the drug is used. The most common effects of heroin addiction include:
- Liver disease
- Skin disease and abscesses around injection sites
- Infections of the valves and lining of the heart
- HIV, Hepatitis B and C
- Chronic pneumonia
- Collapsed, scarred veins
- Blood clots, leading to stroke, pulmonary embolism, and heart attack
- Kidney disease
- Septicemia
- Respiratory depression
- Seizures
- Overdose
- Death
3 Ways to Respond to the Heroin Epidemic
A successful strategy to combat heroin abuse includes prevention, reduction, and treatment. Considering the contributing risks and available resources, three ways to respond, include:
1. Ensure Appropriate Prescribing of Opioid Painkillers
The strongest risk factor for heroin addiction is the existing addiction to prescription opioids. Offer providers with the appropriate education on best practices for effective screening, drug history analysis, and painkiller prescribing alongside resources, such as prescription drug monitoring programs to identify high-risk individuals early and improve prescribing practices.
2. Increase Access to Medication-Assisted Treatment (MAT)
Per SAMHSA, “Medication-Assisted Treatment is the use of FDA- approved medications, in combination with counseling and behavioral therapies, to provide a “whole-patient” approach to the treatment of substance use disorders.” Although MAT has proved to be clinically effective, the treatment is greatly underutilized due to the misconceptions of substituting one drug for another and negative perceptions of MAT in communities. The goal of MAT is full recovery for the individual to live autonomous life.
3. Expand Administration and Use of Naloxone (trade name: Narcan)
Naloxone is a medication used to reverse the effects of heroin. When given intravenously, Naloxone works within 2 minutes, and when injected into muscle, works within 5 minutes. Multiple doses may be required as the duration of action of most opioids is greater than that of naloxone. When given to opioid dependent persons, it may cause symptoms of opioid withdrawal. Small doses administered every few minutes until the desired effect is reached may prevent withdrawal symptoms. By expanding naloxone use, providers can reduce heroin overdose deaths
Final Thoughts
According the Substance Abuse and Mental Health Services Administration (SAMHSA)’s National Survey on Drug Use and Health (NSDUH), in 2016, over 11 million Americans misused prescription opioids, nearly 1 million used heroin, and 2.1 million had an opioid use disorder due to prescription opioids or heroin. Success requires a multi-pronged approach encompassing providers across the continuum of care. Ensure that your providers have access to education on risk assessment to provide proactive care and avoid unnecessary and costly utilization and continuously build competency on prescribing best practices and alternative treatment options.
Opioid Crisis Solutions
Learn more about tackling the opioid and heroin crisis head-on.
Learn More →





