Over 42 million people are food insecure in the United States – that’s approximately 1 in 8 people. 1 in 4 adults in the United States have two or more chronic health conditions.
A recent study by the Economic Research Service on food security and health among working-age adults showed strong correlation between food security and chronic health conditions. Households that are food secure have access all the time to the types and quantities of food needed for all household members to enjoy an active, healthy life. Households that have low food security must make decisions such as skipping or cutting meals because there is not enough money for food, eating unbalanced meals because it is more affordable, or not buying more food when it runs out because the household needs to get money first.
If We Solved Food Insecurity, How Would This Affect Diabetes Management and Chronic Disease Treatment?
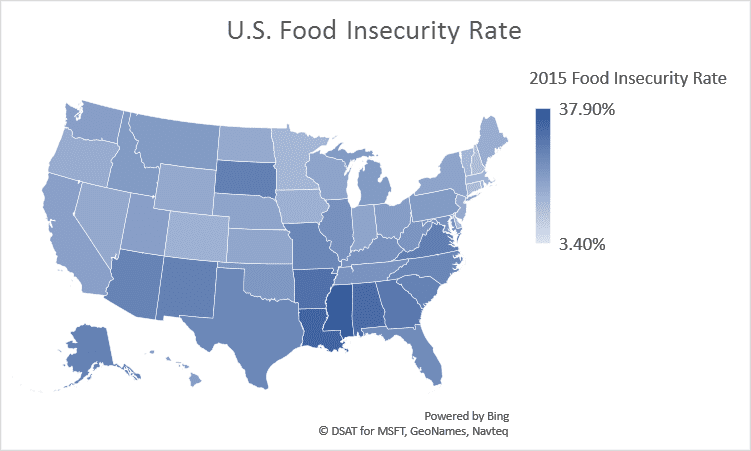
Date from Feeding America.
The following thought exercise will use the correlation between food security and chronic diseases to explore what could happen in the healthcare setting if we solved food insecurity. The major assumption made here is that food security levels impact the incident rate of diabetes. I will also address how doctors in our current environment can address food insecurity on patient- and population-levels to get us to a food secure world.
Suppose the number of patients with diabetes reduces as the U.S. becomes food secure. With few incidents of diabetes, doctors would see the number of patients with diabetes drop, the hours they spend with patients with diabetes will drop, and the percentage of revenue tied to caring for diabetes would also reduce.

Additional implications:
- This means doctors will have more time to spend with their other patients. Patients only remember about 49 percent of the information their doctors give them without prompting. There is consensus among physicians about the importance of patient-centered medicine. However, time pressure is a major obstacle preventing physicians from incorporating the techniques shown to improve patient engagement. With more hours to reallocate, doctors could put techniques like agenda setting, teaching back, discussing multiple options, asking open-ended questions, eliciting patient preferences to practice. This could possibly help the healthcare industry reorganize to create systems that give providers the time to use these strategies effectively.
- While cost is one of the measures of health care performance, time spent by providers on specific tasks and conditions is also a measure of improvement. With more time available to spend with patients, it is possible that patients with other chronic diseases will be better equipped to manage their care and further reduce the number of chronic disease incidents. Patients with ambulatory needs could also have higher patient satisfaction and care quality now that physicians have more time to incorporate preventative care, social determinants of health, patient education, and customer service into their care.
- As the quality of care and patient satisfaction increases, doctors’ value-based reimbursement rates would also likely increase for most patients and conditions treated. Also with more time, doctors may be more likely to participate in value-based care learning and practice to continue improve care quality and lower health care costs.
What Can Health Care Professionals Do Today to Move Us Further along Eliminating Food Insecurity?
Food insecurity refers to the lack of available financial resources for food. It impacts every community in the United States. It is a problem multiplied by overlapping issues like housing, social isolation, education level, medical costs, and low wages.
The food insecurity rate in the U.S. ranges from 3.4 percent to over 35 percent in some counties. According to 2015 data from Feeding America, the county with the highest rate of food insecurity is Jefferson County, Mississippi where of the approximately 2,720 people experiencing food insecurity. 18% are above the nutritional program threshold – which means they may not qualify for state/federal nutrition programs but could benefit from other community resources to fill food gaps. The county with the lowest rate of food insecurity is Grant County, Kansas where of the approximately 340 people who are food insecure and 92% of which are below the SNAP threshold of 130% poverty.
Step 1:
The first step is bringing up the level of awareness of food insecurity and reduce stigma to using resources. When health centers know about the food insecurity rate of their service area, they can develop and refine the path from screening to assistance services.
- Both patients and clinicians need to understand how food insecurity harms and lead to costly impacts on health and well-being. Clinicians can easily create a chart of community organizations, state and federal programs for patients to take part of if they are facing food insecurity.
- 83 percent of individuals who qualified for SNAP benefits received them in fiscal year 2015. Many people avoid assistance programs for various reasons, but as a trusted source of advice, clinicians can emphasize the benefits to the patients’ health and steer them to the available resources that will help stretch limited food dollars.
Resources |
|
Community |
|
State/Federal |
|
Step 2:
The second step is identifying which of your patients could benefit from additional resources. Clinicians can identify which patients are at risk of or experiencing food insecurity by using the Hunger Vital Sign into their screening workflow. Developed in 2010, the Hunger Vital Sign is a 2-question screening tool based on the US Household Food Security Scale to identify young children in households at risk of food insecurity. It has since been added into the Accountable Health Communities Screening Tool by the Centers for Medicare and Medicaid Services. The two questions are:
- “Within the past 12 months we worried whether our food would run out before we got money to buy more. Was that often, sometimes, or never true for you?”
- “Within the past 12 months the food we bought just didn’t last and we didn’t have money to get more. Was that often, sometimes, or never true for you?”
Step 3:
Lastly, doctors, nurses, and other health care professionals can build cross-sector partnerships and align with advocacy efforts to affect policy decisions that affect most people’s health. This could include raising awareness about food insecurity and the necessity of a strong nutrition safety net to end food insecurity, fund the emergency food system, and strengthen nutrition programs. In 2015, a FQHC in rural Kentucky started sending 125 patients and their families to farmers’ markets with vouchers to purchase fresh fruit and vegetables. By 2017, all together, the patients lost 105 pounds, their glucose levels dropped by a cumulative 267 points, and their blood pressure levels improved by 25 percent. This benefits the patients, the local farming economy, the health center and payers.
In Cosmos, Carl Sagan wrote, “Imagination will often carry us to worlds that never were. But without it we go nowhere.” This thought makes sense for an astrophysicist looking at galaxies light years away that may no longer exist by the time the light reaches us. But imagining realities into existence is something we do daily. We plan, make goals, and dream every day. So, let us add into our plans for a healthy population where social determinants like food security are met and prepare for the new challenges.
Interested in more resources that explore how social determinants effect health? Learn more.






