As the nation contended with the coronavirus pandemic, existing health and healthcare disparities among Americans became exacerbated. While anyone could be infected and develop COVID-19, it became increasingly apparent that traditionally marginalized populations—including people of color—were much more likely to contract and die from this disease. The reason behind these discrepancies lies in understanding the intersectionality of social determinants of health (SDOH) and COVID-19.
SDOH are the conditions in which people are born, live, and age that affect a wide range of health outcomes. There are many things that could be considered SDOH, but Healthy People 2020 categorizes these conditions into five groups:
- Economic stability—this includes issues like poverty, employment (including becoming unemployed or underemployed), and food or housing insecurity.
- Education—this includes variables like high school graduation rates, literacy levels, and access to early childhood education.
- Health and healthcare—this category includes access to healthcare, access to primary care, health literacy levels.
- Neighborhood and built environment—this includes access to healthy foods, quality of housing, and neighborhood crime and violence rates.
- Social and community context—this category includes issues such as discrimination, civic participation, and incarceration.
Impact of social characteristics on healthcare access
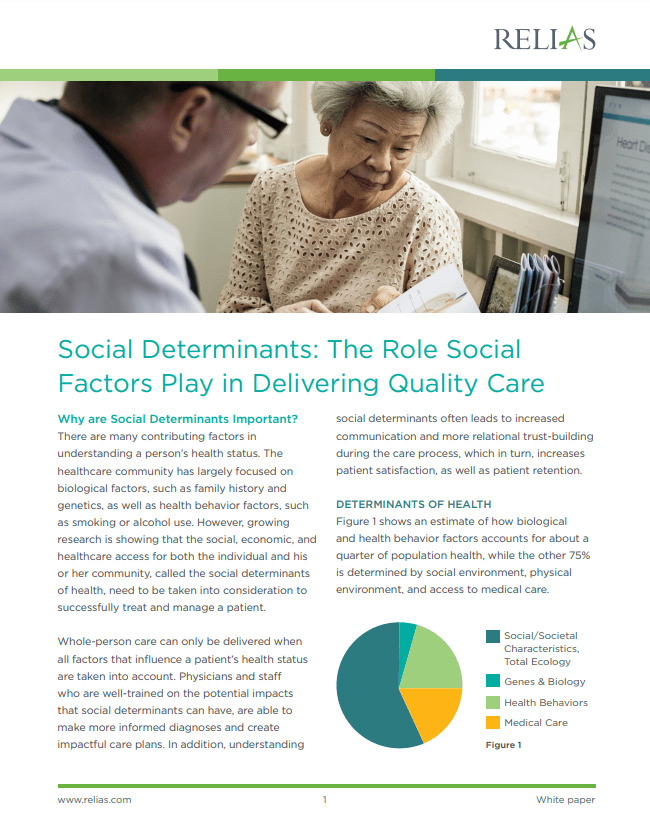
Of course, biological/genetic factors as well as health behaviors also have a hand in an individual’s or population’s health outcomes. However, these factors only account for about 25% of health outcomes. In contrast, social characteristics, access to healthcare, and physical environment account for the other 75% of health outcomes. In other words, social determinants of health drive the vast majority of our wellness and health outcomes.
Despite this, individuals’ health behaviors take the brunt of the blame. During the pandemic, a state senator from North Carolina suggested that the coronavirus hit the state’s Latino population harder because they do not practice social distancing or wear masks as frequently as other groups. An Ohio lawmaker made similar remarks about Black Americans, stating that this population experienced a higher rate of coronavirus cases because they do not wash their hands as well as other groups. It is critical to point out here that many individuals—including policymakers—will often attribute individual behavior, rather than systemic causes, when trying to explain health disparities.
When viewed from the lens of social determinants, there are many reasons outside of individual behavior that better explain why Black and Latino Americans died of COVID-19 at substantially higher rates than white Americans during the pandemic.
Economic stability
25% of Black and Latino workers are employed in the service industry and considered essential workers, which left them at a higher risk of contracting the coronavirus. Additionally, these essential worker positions are much less likely to have benefits such as paid sick leave, leaving individuals in the difficult predicament of going to work even if they have symptoms, when staying home could mean losing days’ or weeks’ worth of wages.
Neighborhood and built environment
Black and Latino Americans are much more likely than white Americans to live in multigenerational households. This can make it much more difficult to appropriately socially distance if a family member falls ill.
Social and community context
Black and Latino individuals are largely overrepresented in jail, prison, and detention center populations. These settings carry a large risk for infection due to:
- Congregate living
- The inability to socially distance
- Poor access to adequate healthcare
Social determinants of health and COVID-19
These are just a few examples of the social determinants that impacted Black and Latino individuals’ health outcomes during the COVID-19 pandemic. There are many more aspects of SDOH that could also come into play. But what these clearly demonstrate is that, overwhelmingly, social determinants had a heavier hand in the poor outcomes among these populations during COVID-19 than among other populations. These are just a few examples of the social determinants that impacted Black and Latino individuals’ health outcomes during the COVID-19 pandemic.
When employers, agencies, and healthcare organizations begin to understand the nuance of social determinants and the effect they have on COVID-19 infection and death rates, they can better understand how to help individuals prevent this disease. It can also help providers identify different at-risk groups in their community and drive them to provide targeted and individualized outreach to high-risk populations. As the pandemic continues, understanding the connection between SDOH and COVID-19 is one of the best ways providers can address the needs of high-risk populations and begin to initiate activities that will prevent infections and deaths.
Social Determinants: The Role Social Factors Play in Delivering Quality Care
Whole-person care considers more than just presenting symptoms, but considers factors such as patient education, income, and access to transportation. Learn how to take these factors into consideration to successfully plan care for patients and improve outcomes and patient satisfaction.
Download the White Paper →





