Pregnancy today is often portrayed as a fun adventure that begins with clever social media announcements, cute gender reveal parties, and finally, the highly anticipated first baby photo. And while, yes, people freely talk about the not-so-glamorous symptoms of morning sickness, fatigue, and heartburn, we fail to mention the anxiety and worry that comes with carrying a baby. What’s perhaps chalked up as being hormonal or overly emotional is often simply the incredibly valid concern that pregnancy is hard.
I learned this all too well early in my pregnancy journey. I’d always found it nerve-wracking to imagine my life as a mother, when I couldn’t definitively know if it was even possible for me. I was reaching the age where several of my friends were having trouble conceiving, and I couldn’t help but wonder if I would struggle as well.
Before we welcomed my first daughter, I suffered two early miscarriages – an experience I only then learned was relatively common. As I discussed my struggles with others, the less alone and more hopeful I felt. Still, I couldn’t help but wonder why the reality of miscarriages seemed like a taboo topic.
As much as I tried to relax throughout my pregnancy as it progressed, it felt next to impossible. There was an unexplainable pressure I felt to keep my baby healthy, without knowing what I should or shouldn’t do differently. I became frustrated when others would offer advice to be careful not to stress out too much (it wasn’t good for the baby) or to keep my mind busy on other things. Easier said than done.
Pandemic Pregnancy
After my daughter’s first birthday, I learned I was pregnant again, but I instinctively knew something wasn’t right. Because this was now my third loss, my OB/GYN ordered lab work and I learned I had two factors working against me – a rare blood clotting disorder and a mutation in the MTHFR gene – both associated with pregnancy complications. Relieved to at least have some answers, I discussed my options with my OB/GYN in planning for a second baby.
Needless to say, my next pregnancy was pretty stressful. I knew the first 12 weeks were the riskiest in terms of miscarrying, but I felt little relief even after hitting that milestone. Despite doing everything I could to promote a healthy pregnancy (a daily blood thinner injection and supplements), I knew only so much was in my control. Instead of sharing my exciting news with friends and family, I felt pressured to hide the fact that I was pregnant – as though I would jinx it with every new person we told.
By Christmas I was nearly six months pregnant and the emergence of the novel coronavirus was starting to fill my newsfeed. Within weeks, it had arrived in the U.S. and I began to panic. Throughout my pregnancy, I had relied on data and research to get me through the “unknowns” only now I had nowhere to turn. There was little my doctor could tell me that I hadn’t already read, and in my final checkup appointments she sat across the room from me and no longer felt safe offering her hand to help me out of the exam chair.
What had been my countdown to relief became a new and unfamiliar stress. If cases were beginning to rise, how bad would things be in the coming weeks? Preparation becomes a coping mechanism for moms to be, but how can you prepare for something you could never see coming?
Delivery on Lockdown
Because my pregnancy was considered high-risk, we had a scheduled C-section at the end of March. The hospital’s protocols were changing day by day, and I knew it was a possibility that I might have to deliver without my husband. I had worked in healthcare communications on maternal safety projects, and I knew the risks associated with C-sections and maternal mortality, even before the added stress of the pandemic. At this point in a pregnancy, most women are eager to get to the hospital and meet their baby, but I was a bundle of nerves. If someone had given me the option of a natural home birth, I would have taken it hands-down out of fear of the virus’s exposure in the hospital.
On the morning of our scheduled delivery, we joined a line of other patients to have our temperatures checked and asked a series of questions about our recent travel, possible exposure, etc. Before surgery, my nurse informed us that my husband would be the only person allowed in our room, and if he had to leave for any reason, I would be on my own. Our C-section went well, and we welcomed a second baby girl hours later. With every shift change for the remainder of our stay, protocols were changing, and on our second day, we were confined to our room. As our fears and anxieties grew, we insisted on leaving the following day, even though I knew it would be physically challenging post C-section.
Before leaving the hospital, we talked with the house pediatrician and went over the typical details, but were mostly consumed with the million-dollar question – how do you care for a newborn during a pandemic?
The New Normal Paradox
I’m forever grateful for my two daughters, however hard and unpredictable our journey may have been. And while they’re young enough to not be as obviously affected by COVID-19’s restrictions or lockdowns as other kids, the parental worry is no less.
The experiences between my daughters’ births were night and day, and nothing can ever change that. Many of my relatives haven’t met or held our newest daughter – my grandfather will now never have the chance – and we’ll never get that time back. It’s an uncomfortable reality to know that my tiny daughter, who I went through so much with to get her here safely, is at a higher risk of exposure with anyone who cares for her other than me, making me less inclined to take time for myself (even when I know I need it).
But, like most, I’ve found the silver linings in the invaluable family time at home. And while my younger daughter is a complete and total homebody, I have been able to bond with her in a way that wasn’t possible with our first.
With so many uncertainties remaining for the expecting moms out there, it might be helpful to know that someone can empathize with all their stress and worry – even as they celebrate the joy of a new baby. It’s always OK to acknowledge the pressure that comes along with pregnancy, especially now.
It can’t be said enough – front-line caregivers are selflessly risking their lives to care for patients during this pandemic. The care and compassion I received made our birth during COVID-19 seem somewhat normal, and I nominated three of my nurses for The DAISY Award® as a small token of my gratitude. Last year, the World Health Organization designated 2020 as the International Year of the Nurse and the Midwife, and that will always carry a special meaning for me.
I always knew my work experience with maternal safety projects would play into my journey through pregnancy and motherhood, and I felt empowered through the knowledge I’d gained over the years. Patient education is an extremely powerful tool in improving care for mothers and their babies, and enables patients to better advocate for their care (myself included).
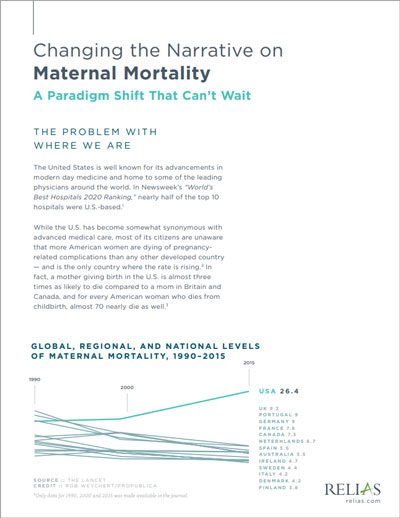
Changing the Narrative on Maternal Mortality: A Paradigm Shift That Can't Wait
Due to the lack of progress from our nation’s hospitals and health systems, many quality organizations have intervened to set standards and requirements in place that will ensure hospitals and health systems follow best practices to rapidly and drastically affect mothers’ and babies’ care. This white paper outlines where we are as a nation, where we need to go in terms of improvement, and most importantly — how to get there.
Download the White Paper →





