State legislatures have passed numerous bills to address the opioid crisis, ranging from the most common legislation – allowing persons to administer opioid antagonists without fear of arrests and other penalties – to distinctive restrictions, such as Kentucky’s limiting the maximum opioid drug prescriptions to three days.
Indiana signed eleven pieces of legislation to address the lack of treatment centers and permit projects that will treat specific vulnerable populations, such as women with newborns and people with non-violent drug convictions. Pennsylvania passed five pieces of legislation to establish safe prescribing curriculum, limit emergency and urgent care center opioid prescriptions to seven days, restrict ability to prescribe opioids to minors, require law enforcement agencies, health centers and pharmacies to serve as drop-off locations, and require prescription data to be input to the monitoring program within 24 hours.
According to the Centers for Disease Control and Prevention (CDC), the five states with the highest rates of death due to drug overdose in 2015 were West Virginia (41.5 per 100,000), New Hampshire (34.3 per 100,000), Kentucky (29.9 per 100,000), Ohio (29.9 per 100,000), and Rhode Island (28.2 per 100,000). Four of these hardest hit states have passed prescription limits (NH, KY, OH, RI). Three of the five have passed Continuing Medical Education requirements related to pain management and the prescription and distribution of controlled substances (NH, RI, WV).
According to the CDC, the five states with the highest rates of death due to drug overdose in 2015 were West Virginia, New Hampshire, Kentucky, Ohio, and Rhode Island.
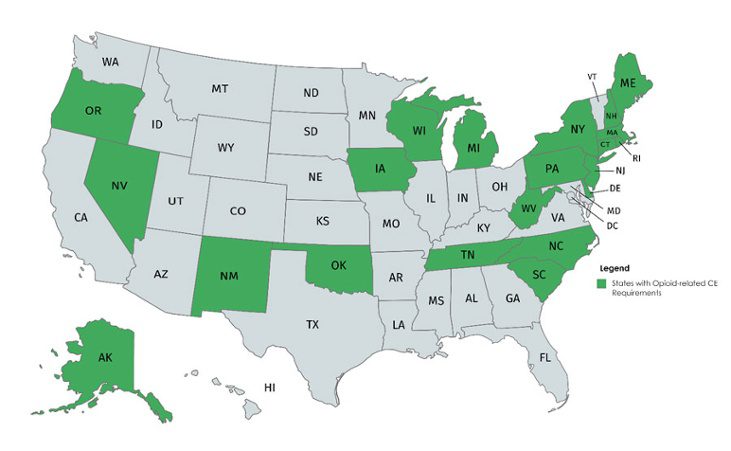
States Requiring Opioid Crisis-Related CMEs
Continuing medical education or CMEs are “educational activities which serve to maintain, develop, or increase the knowledge, skills, and professional performance and relationships that a physician uses to provide services for patients, the public, or the profession (ACCME).” In total, there are 23 states requiring CMEs related to pain management and opiates. These states, along with the rest of the states, are also scrambling to pass legislation to address the opioid crisis.
While almost half the country’s states have required opioid-related CMEs, the requirements are far from standard. They differ in three main ways: clinician role, hours required, and renewal periods. In New Jersey, you could be required to complete 1.0 to 6.0 hours of educational programs on prescribing opioids depending on whether you are a pharmacist, a certified nurse midwife, or an advanced practice nurse. In Connecticut, prescribers and distributors are required to take 1.0 hour of training or education, while Pennsylvania requires 4.0 hours (separated into 2.0 hours in pain management or identification of addiction and 2.0 hours in prescribing or dispensing opioids). New Mexico requires 5.0 hours on a triennial basis, while West Virginia requires 3.0 hours on a biennial basis. Iowa requires 2.0 hours of chronic pain training every five years. The wide range of variation makes it difficult for providers to support their staff’s compliance requirements.
There is effort in Congress to address the opioid crisis through training on pain management and treatment. The Opioid Preventing Abuse through Continuing Education Act (Opioid PACE Act, House Resolution 2063) was introduced in April 2017 by Representative Schneider, IL to amend the Controlled Substances Act and mandate 12.0 hours of training once every three years for prescribers and dispensers. The training may be completed in a classroom setting, through seminars at professional society meeting, electronic communications, or other forms approved by various organizations approved by the Secretary of Health and Human Services. It must cover topics of pain management treatment guidelines and best practices, early detection of opioid addiction, and the treatment and management of opioid-dependent patients. If passed, the Act would authorize $1 million to carry out the legislative change for 2018-2022.
Create Meaningful CME Courses
As clinicians start taking training to meet the opioid-related CMEs, concerns about the quality and relevance of training should be considered. In conversations with multiple health system executives across the country, all acknowledge that CMEs tend to be taken based on the judgement of clinicians rather than based on the skills that clinicians could improve on and related to the issues in healthcare. As one hospital executive succinctly said:
“Physicians are getting tired of wasting their time with Continuing Education that checks boxes but doesn’t help them at their jobs.”
Medical associations and professionals are pulled in many directions making it difficult to keep track of the most urgent issues in health care and all the ways to tackle the issues. Knowing this disconnection between training and practice, how do we make sure that the quality of opioid-related CME courses will address the problems that clinicians face? The requirement of opioid-related CME emphasizes one major public health issue, but we also need to ensure that the CMEs do not become another check box.
CMEs should help clinicians implement the prescribing guidelines, identify patients who are at risk of developing controlled substance dependencies, and support recovery. If the industry is successful at implementing valuable CMEs that help clinician improve pain management, it would another step towards repairing the breach of trust occurring in the health system and its members.






