Originally known as the Fatal Four (which included aspiration, dehydration, constipation, and seizures), experts in the field of IDD care have identified sepsis as another serious condition for this population. For this reason, the nomenclature has changed to the Fatal Five.
As a member of the Fatal Five conditions, dehydration can affect those with intellectual and developmental disabilities (IDD) more than others. As a direct support professional (DSP), it is crucial for you to learn the signs and symptoms of dehydration, and what to do if your client becomes dehydrated.
By learning how to combat or prevent dehydration in your clients, you can help them achieve a higher quality of life and avoid one of the major health concerns among individuals with IDD.
To that end, let’s review how dehydration presents, why it’s included in the Fatal Five, and what you can do if your client becomes dehydrated.
Why is dehydration included in the Fatal Five?
Dehydration is a minor problem, right?
No, it isn’t. Just ask Marc Carter, whose son Ben has autism. As reported by CNN, Ben refuses to drink from any container other than a specific blue cup. When he didn’t have access to the cup, he experienced dehydration so severe that he required emergency medical treatment. Unfortunately, the manufacturer stopped selling the cup years ago, and Ben’s father feared for his health when they were no longer able to find replacements.
This story has a happy ending: the cup’s manufacturer provided a lifetime supply of cups, so today Ben is happily hydrated. Though the solution to Ben’s problem was a unique one, dehydration is a common and dangerous problem for people with intellectual and developmental disabilities (IDD).
Dehydration simply means that someone doesn’t have enough fluids in their body. Water plays a key role in many bodily functions, and when those functions are disrupted, simple dehydration can spiral into serious problems.
Risk factors for dehydration
People naturally lose fluids all the time through sweat, urine, and other normal bodily functions. Replacing those fluids is what keeps our bodies hydrated. Anything that causes a person to lose extra fluids, or to take in less fluids, can result in dehydration. Common concerns include:
- Vomiting and diarrhea that increase fluid loss.
- Illness, including fever, infections, or other common illnesses can increase the body’s need for fluid while also decreasing the person’s motivation to drink.
- Diabetes can increase fluid output.
- Decreased fluid intake for any reason.
- Excessive exertion or perspiration can increase fluid loss.
- Extreme temperatures – both hot and cold – can cause fluid loss.
- Advanced age reduces a person’s ability to retain water.
- Certain medications increase fluid loss through urination.
- Infants and small children lose fluid more easily than adults do.
These risk factors can be further complicated by disability. For example, many people with IDD experience disruptions in their body’s senses and signals. These individuals might not know they are thirsty. Others may have difficulty communicating thirst or may be unable to get a drink on their own when they need one. Others may have unique behavioral needs, such as Ben’s need for a specific blue cup.
Individuals who can identify thirst and request a drink or get one independently may still have an elevated risk of dehydration. For example, some individuals who require substantial support to use the toilet may see skipping beverages as a solution to other problems. If they don’t have access to a mechanical lift away from home, they may prefer dehydration to either wearing diapers or risking a wetting accident. Others may perceive that their need for support causes a burden on their care providers, so they may reduce fluid intake to reduce fluid output.
Even among individuals with no disability, thirst is easily confused with hunger, and many people do not recognize they are thirsty until they are already dehydrated.
The signs of dehydration
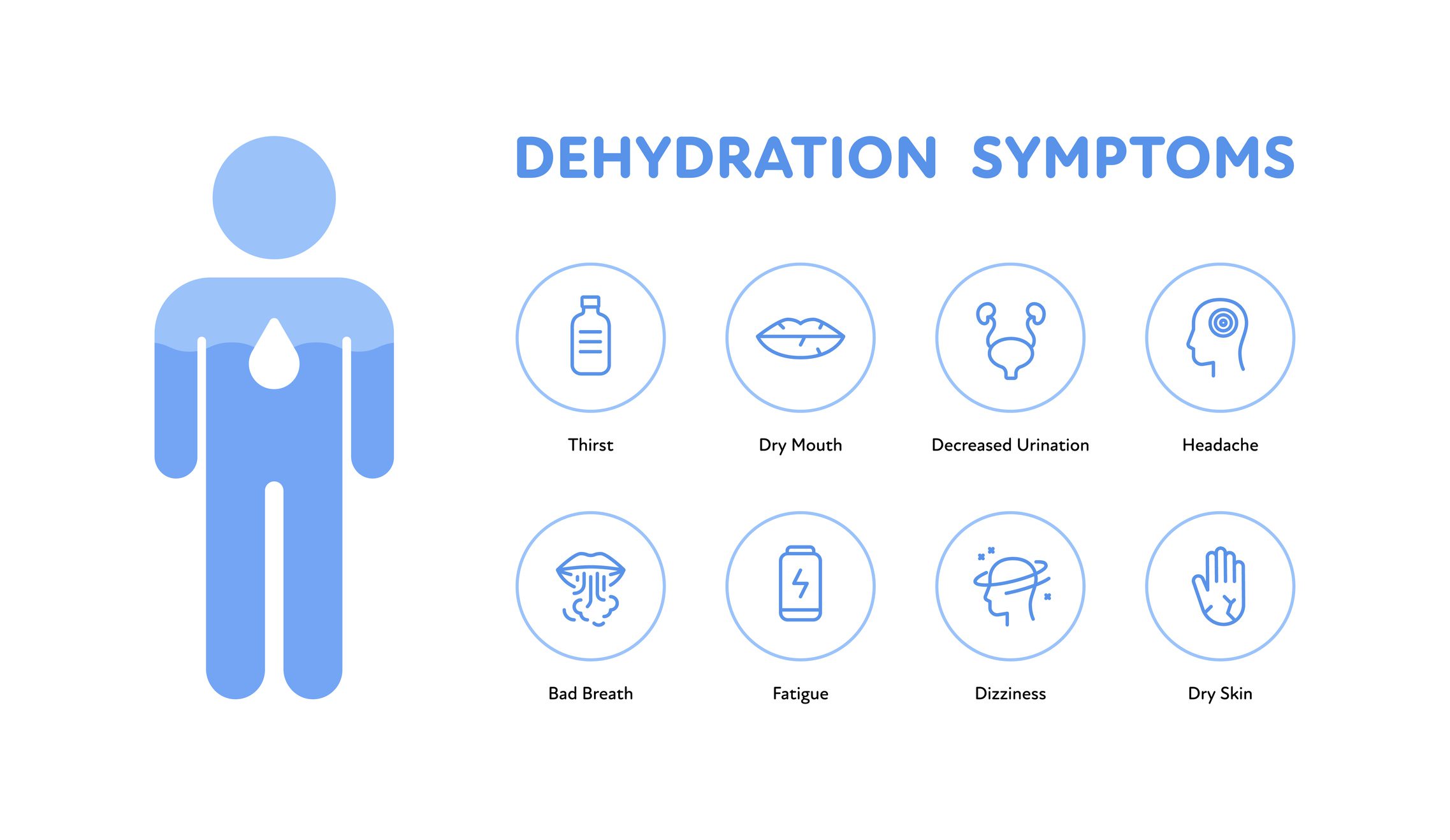
It’s important to monitor the people you support for signs of dehydration. These can include:
- Feeling thirsty
- Dry mouth, tongue, or skin
- Muscle cramps
- Unusual feelings of fatigue
- Constipation
- Headache
- Tiredness or lethargy
- Irritability
- Decreased urine output or dark, concentrated urine
- Dizziness or fainting
- Rapid heartbeat or breathing
- Confusion or disorientation
Note that constipation, another of the Fatal Five conditions, is a symptom of dehydration.
When a person is experiencing mild dehydration, simply drinking more fluids can be sufficient to help them recover. More extreme cases of dehydration may require intravenous (IV) fluids to prevent a medical emergency.
Complications from dehydration
Though dehydration seems simple enough, it can result in serious complications.
- Heat injuries can occur when people are dehydrated, and their bodies overheat. This can be brought on by weather or intense exercise. In its mildest form, heat injury may present as cramps. The most severe form of heat injury, called heat stroke, can be lethal.
- Prolonged lack of fluids can allow bacteria and waste to accumulate in the urinary tract and kidneys. In this way, dehydration can contribute to kidney stones or a urinary tract infection (UTI). UTIs often go undetected and can easily develop into more serious infections.
- Dehydration does not directly cause kidney failure, but kidney stones and UTIs can result in kidney damage or failure if not treated promptly.
- Seizures can result from severe imbalances in electrolytes due to dehydration.
- Dehydration can cause high blood pressure. When experiencing dehydration, blood pressure can drop and then quickly rise in response to this drop.
- In extreme cases, dehydration can reduce the amount of blood in the body, which can put strain on the heart and cause shock. Shock is a dangerous decrease in blood pressure, which can be fatal.
- Dehydration does not directly cause stomach pain. But drinking fluids too fast or taking in fluids with too much sugar in response to dehydration can cause stomach pain.
- Being dehydrated does not make you nauseous, but the complications of dehydration can. Changes in blood pressure, vomiting, and dizziness are all complications of dehydration that can lead to nausea.
- A person is just as likely to become dehydrated in the cold as in the heat, making dehydration in winter a real risk. Make sure to monitor your client’s fluid intake year-round.
- Note that dehydration can contribute to seizures, another of the Fatal Five conditions.
7 ways direct support professionals (DSPs) can prevent dehydration
Because many people don’t feel thirsty until they are already dehydrated, it’s important to drink fluids throughout the day before actually feeling thirsty. Here are seven things that direct support professionals (DSPs) can do to help people stay hydrated.
1. Build routines
Help the people you support build routines, such as having a glass of water after coming home from work or school. When you finish one activity, see if the person you are supporting would like a drink before starting the next. Perhaps they would benefit from carrying a reusable water bottle with them throughout the day? Habits like this can make staying hydrated almost second nature.
2. Be a role model
Offer frequent reminders to drink fluids. If you are feeling thirsty, suggest that you and the person you support get a drink together.
3. Know what counts
Almost any fluid provides hydration, including coffee and tea (contrary to popular belief). Water and low-sugar electrolyte drinks, however, are still best for preventing dehydration.
Additionally, many fruits and vegetables, such as melons, oranges, or cucumbers, contain fluids. Popsicles, smoothies, and similar treats may also contribute to hydration.
4. Beware alcohol and salt
Alcohol and salt in a person’s diet may increase the risk of dehydration. Both impact the balance of electrolytes in the body. Individuals who consume diets high in salt or who choose to drink any amount of alcohol should increase their consumption of hydrating fluids.
5. Be creative
If someone doesn’t like what you have offered, what do they like? Perhaps they prefer carbonation? Fruit flavors? They might prefer their beverages ice cold, or maybe the cold hurts their teeth. Offer a straw, a different cup, or a bottle with a spout. Find what works for the individual you support.
6. Consider consistency
Some people may have trouble swallowing thin liquids and may prefer thicker beverages, such as smoothies. You can also add a thickener to increase the viscosity of the fluids, making them easier to swallow. Note that you may be required to have direction from a medical professional before adding thickener to someone’s beverages. Someone who cannot easily swallow thin liquids is likely at risk for aspiration, another of the Fatal Five conditions, and may require additional supports.
7. Monitor intake
If you are working with someone who can’t manage their own fluid intake, be sure to keep good records to coordinate with the other staff. It’s easy to overestimate the amount of fluids someone has consumed. If the person can manage their own fluid intake, help them find a way to track it visually. There are many phone apps that help with this, or you can always make a paper chart.
Final thoughts on dehydration and the Fatal Five
Dehydration should not be taken lightly. These tips will help you prevent a dangerous condition before it starts. Recognizing the risk factors for dehydration and acting proactively today could prevent a hospitalization tomorrow.
DSPs and other caregivers need to know how dehydration and the rest of the Fatal Five – aspiration, constipation, sepsis, and seizures – interact and potentially cause other serious health problems. The only way to keep the Fatal Five from claiming more lives is education and prevention.
To learn more, be sure to read our posts on the other four conditions in the Fatal Five:
Fatal Five Posters
Relias created these posters on The Fatal Five to help you educate your employees and protect the people you serve. Print out these posters on legal-sized paper, hang them in your offices and facilities, and save lives.
Download the Posters →