While we don’t yet have complete data from the first year of the Patient-Driven Groupings Model (PDGM), we are starting to see a clearer picture of best practices for home health claims. Pay attention to the details to ensure that your home health agency receives all the Medicare reimbursements you are due.
When the Centers for Medicare and Medicaid Services (CMS) instituted the payment model in January, no one could anticipate the upheaval caused by the COVID-19 pandemic. CMS granted temporary waivers for some requirements as the pandemic intensified. But by now your organization should be prepared to work within the PDGM framework.
Diagnoses Drive PDGM Payments
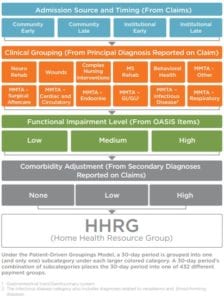
With PDGM, case-mix adjustments rely more heavily on patient characteristics, rather than volume of services, to accurately pay for home health services. CMS began using the model to calculate payments for the Home Health Prospective Payment System for periods of care beginning January 1, 2020.
Structure of the Patient-Driven Groupings Model
PDGM differs from the previous fee-for-service model in three main ways:
- Incentive is applied to health optimization instead of use of services.
- Quality is often factored into the payment.
- Providers are encouraged to collaborate.
To ensure you receive all Medicare funds you qualify for, analyze your reimbursement trends to determine where payments have come up short. Once you know your organization’s billing weak spots, consider the strategies we share here for working effectively with PDGM.
Best Practices in Referral and Intake
Added pressures from COVID-19 have exacerbated intake challenges. Common issues include missing information in referrals, hard-to-reach referral sources, and gaps in staff knowledge about clinical groupings.
To shore up your referral and intake process:
- Assist in eliminating questionable encounter diagnosis.
- Implement scripting for intake staff.
- Enhance training and coaching on ICD-10 use.
It will help to use a checklist during the intake process. Yours should include:
- An accurate referral source.
- Home health principal diagnosis.
- Physician face-to-face encounter and supporting documentation.
- Patient secondary diagnosis information for comorbidities.
- Requested services.
- Supporting documentation from referring physician and facility.
Best Practices for Admissions
Clear procedures and expectations will help your admissions team maximize compliance. Tips for setting admissions targets include:
- The goal should be new patient acceptance within four hours of referral.
- Acceptance of new patients is a joint decision between intake and clinical leaders.
- Potential decisions not to take under care should escalate to clinical leadership.
- Start of care and admission visit should be scheduled and occur within 48 hours of referral acceptance.
- OASIS, assessment, and plan of care should be completed within 48 hours.
Best Practices for Evaluating Functional Impairment
Experience and education are vital for clinicians diagnosing and developing plans of care for individuals in home health.
- Ensure the clinician conducting the assessment has OASIS training (and ideally a certification, such as COS-C, which is the Certificate for OASIS Specialist-Clinical).
- Consider current functional status assessments as you develop the plan of care. Look for outcome performance improvement opportunities.
- Identify patterns of internal referral and use of rehabilitation therapy services. Look for opportunities to change those patterns using strategies that have worked. For example, if occupational therapy has demonstrated positive outcomes with this type of functional impairment with other patients, consider that as part of the current plan of care.
- Functional status changes from the first to second 30-day period are considered a significant change in condition (SCIC). An SCIC requires a clinician to conduct an OFA, or other follow-up assessment.
Best Practices for Coding Diagnoses
The principal diagnosis code reported on the claim must fit into one of the 12 PDGM clinical grouping categories to be eligible for the Medicare home health benefit. Similarly, make sure to report any comorbidities, as they can affect resources use and reimbursement. CMS has grouped comorbidities for home health into broad clinical categories that the agency will consider for payment adjustment.
Be careful to avoid using principal diagnosis codes that CMS deems vague, unspecified, or not allowed. If you use one of these codes for the primary diagnosis, CMS will return the claim for more definitive diagnosis coding.
If a diagnosis from a referring provider does not fit a clinical grouping under PDGM, the diagnosis may need to be more specific. For instance, a primary diagnosis of “muscle weakness, generalized” is an unacceptable principal diagnosis code for home health services. If the patient’s diagnosis is coded this way, the home health clinician will need to probe for the reason for muscle weakness. Then the clinician can provide a more detailed diagnosis, such as “muscle wasting and atrophy of the right lower leg,” that aligns with home health care eligibility.
Note that if the primary diagnosis changes in the first 30-day period, you will need to indicate it on the second 30-day period claim.
One way to deal with the returned claims problem is to look at the top five questionable encounter codes you are using. With your team, plan and practice how to eliminate the use of those codes by finding appropriate alternatives.
Home health agencies seem to be giving close attention to accurate coding, as early reports indicate CMS is categorizing few claims as questionable encounters.
Use of Therapy Services Under PDGM
Even before the coronavirus pandemic, home health agencies responding to PDGM decreased their therapy utilization, as therapy service thresholds no longer applied.
With a few more weeks left in 2020, final therapy utilization data is not available. Of course, therapy plays a significant role in patient outcomes. So we’re all looking forward to reviewing the 2020 therapy utilization data under PDGM.
Marking a shift in procedures and roles, PDGM now allows reimbursements if therapy assistants provide maintenance therapy. Therapist assistants can perform maintenance therapy services under a program established by a qualified therapist.
The qualified therapist is still responsible for:
- The initial assessment.
- The plan of care.
- Maintenance program development and modifications.
- Reassessment every 30 days.
- Supervision of the therapist assistant.
The Details and the Big Picture
In summary, you must pay close attention to all segments of the PDGM structure to ensure smooth processing of your home health claims. By getting the picky details right, you can step back and see a favorable broader view for your organization’s CMS reimbursements.
Many of us are anxious to put 2020 and its health challenges behind us. We’d rather not dwell on them. However, if you look back with insight into your PDGM practices, you’ll be able to see a better way forward for your team and your clients in 2021.

Patient-Driven Groupings Model Toolkit
To help your organization maintain compliance with PDGM, we have put together a resource toolkit that contains white papers, webinars, guides, and more.
Download the Toolkit →