September is National Suicide Prevention Month, when mental health advocates, prevention organizations, survivors, allies, and community members unite to promote suicide prevention awareness. Relias is one such ally. We admire the strength of our clients who work daily to help prevent suicide and are committed to supporting other organizations doing the same.
Relias is participating in National Suicide Prevention Month through September and beyond, by sharing helpful information, tools, and resources across a variety of settings so that we can help to meet the needs of individuals where they live, work, and learn.
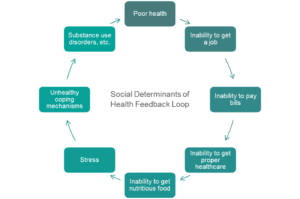
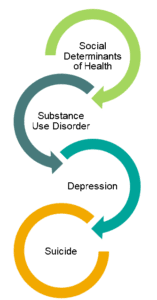
The rate of suicide in the U.S. has risen by 30% over the past 20 years. As a care professional in the human services industry, you’re most likely familiar with the common risk factors and warning signs for suicide, but there are other important factors to consider, like social determinants of health (SDOH) which play a large role in substance use disorders (SUDs) and depression.
These determinants feed off one another and produce a downward spiral effect that can increase the risk of suicide. It is important for you to become familiar with SDOH and their impact so they can better inform the way you provide care — and possibly save lives.
Social determinants of health
Determinants of health include the availability of health care, individual behavioral choices, and biological and genetic factors. A subcategory of this was created called social determinants of health, which the World Health Organization defines as “the conditions in which people are born, grow, live, work, and age” that are “shaped by the distribution of money, power, and resources at global, national, and local levels.”
Social determinants of health contribute to health disparities among various groups of people based on gender, race, and socioeconomic status. They are also an underlying factor in the development of major health concerns in the U.S. including obesity, heart disease, and depression.
There are complexities that exist within these social determinants of health that cause a feedback loop of hardship, as shown in the diagram below. It is easy to see how each hardship can lead to the next, finally resulting in unhealthy coping mechanisms, such as substance use disorders.
Substance use disorders, depression, and the downward spiral
Just like with overall heath, there are social determinants of suicide. As explained above, one major determinant is unhealthy coping mechanisms, including SUDs. Compared with the general U.S. population, people with substance use disorders have a 10 to 14 times greater risk of death by suicide, and more than 50% of individuals who die by suicide suffer from major depression.
Left unattended, the feedback loops for SDOH, SUDs, and depression overlap, forming a tightly interlocked relationship that creates a downward spiral. A person experiencing a substance use disorder who can’t seem to get out of the loop becomes hopeless. Hopelessness may lead to worsened depression, which could then lead to thoughts of suicide and possibly dying by suicide.
How to address the social determinants of suicide
To properly address the social determinants of suicide, organizations can engage in activities that both directly and indirectly improve the mental health of their clients. To directly impact their clients, organizations can conduct assessments to determine how clients are impacted by the social determinants of suicide, as well as their risk of dying by suicide.
To indirectly impact their clients’ mental health, organizations should build strong relationships with other institutions in the community that work with issues around housing, food security, and more. Additionally, your organization can petition local, state, and federal governmental representatives to put greater emphasis on finding solutions to social determinants of suicide.
The importance of assessments
There are several resources available to help prevent suicide, but it is critical that we use those resources collectively, across a wide variety of settings. We need a comprehensive approach to suicide prevention that meets individuals where they are. Ensuring your colleagues and staff are properly trained on how to identify suicide risk factors and how to intervene when risk is present are important steps in preventing suicide.
Factors such as food insecurity, financial stress, job loss, and more contribute to deaths by suicide. A study conducted by the Department of Veteran Affairs found a “a significant positive relationship between a positive screen for housing instability and a Veteran having a diagnosis of post-traumatic stress disorder (PTSD), depression, psychosis, alcohol abuse, drug abuse, and previous suicide attempt or intentional self-harm.”
Clinicians, counselors, social workers, and others within your organization need to receive training on how to properly screen for these stressors.
A basic screening for social determinants of suicide should include questions such as:
- Do you worry that you will run out of food?
- Do you have a place to live or are you worried about losing your housing?
- Do you feel safe, both physically and emotionally, where you live?
- Do you have a reliable means of transportation to get to and from work?
As an organization, making sure your staff receive the proper training on administering these assessments can go a long way to improving the care you give to your community and lowering the rate of death by suicide.
Developing relationships with other organizations
If directly combating the social determinants of suicide (e.g., hunger, housing loss, etc.) lays outside your organizational scope or ability, partner with other organizations in your area that directly work with these issues. This could include working with a local food bank or food pantry, your area’s Habitat for Humanity branch, or transportation agencies.
By providing your clients with greater access to food, transportation, housing, and other means, you’re helping to increase their quality of life, which, in turn, can reduce the risk of suicidal ideation.
As stated by Rola Aamar, PhD, Senior Consultant for Clinical Effectiveness at Relias:
“Access to community supports including homeless shelters, job training and placement organizations, food shelters, transportation services, and community centers can help you provide clients with direct connections to the resources they need to improve their quality of life.”
Using advocacy to fight the social determinants of suicide
According to the Black Dog Institute, data exists that shows the link between governmental policy and suicide rates. These factors include LGBTQ marriage equality laws, welfare policies, firearms legislation, and ease of obtaining alcohol.
As an organization, you can petition your local, state, and federal representatives to take action on these social determinants of suicide. By instituting policies that affect people’s wellbeing during times of economic hardship, access to lethal means, and equality before the law, these government representatives can make a positive difference in suicide prevention.
Write letters, tweet at your local politicians, and encourage others in your community to do the same. By taking action in the public sphere, your organization can make an impact in the fight to reduce the social determinants of suicide.
If you are in crisis or know someone who is, please call or share the National Suicide Prevention Lifeline at 1-800-273-TALK (8255), or contact the Crisis Text Line by texting TALK to 741741.

Suicide Prevention Training
Relias provides suicide screening, assessment, and treatment training for all employees, whether direct care, support, administrative or supervisory staff.
Learn More →