The healthcare revenue cycle is important for every hospital and healthcare practice. Accurate medical coding has a big impact on revenue cycle management (RCM), but it is not the only factor affecting its success. Additional key performance indicators (KPIs) can help you measure whether your healthcare revenue cycle is both efficient and effective.
The revenue cycle includes all processes from capturing a patient’s information to final billing and payment. “Oftentimes, we see revenue cycle treated as a department that sits on the back end with billing,” said Melissa Scott, director of advisory services at Change Healthcare.
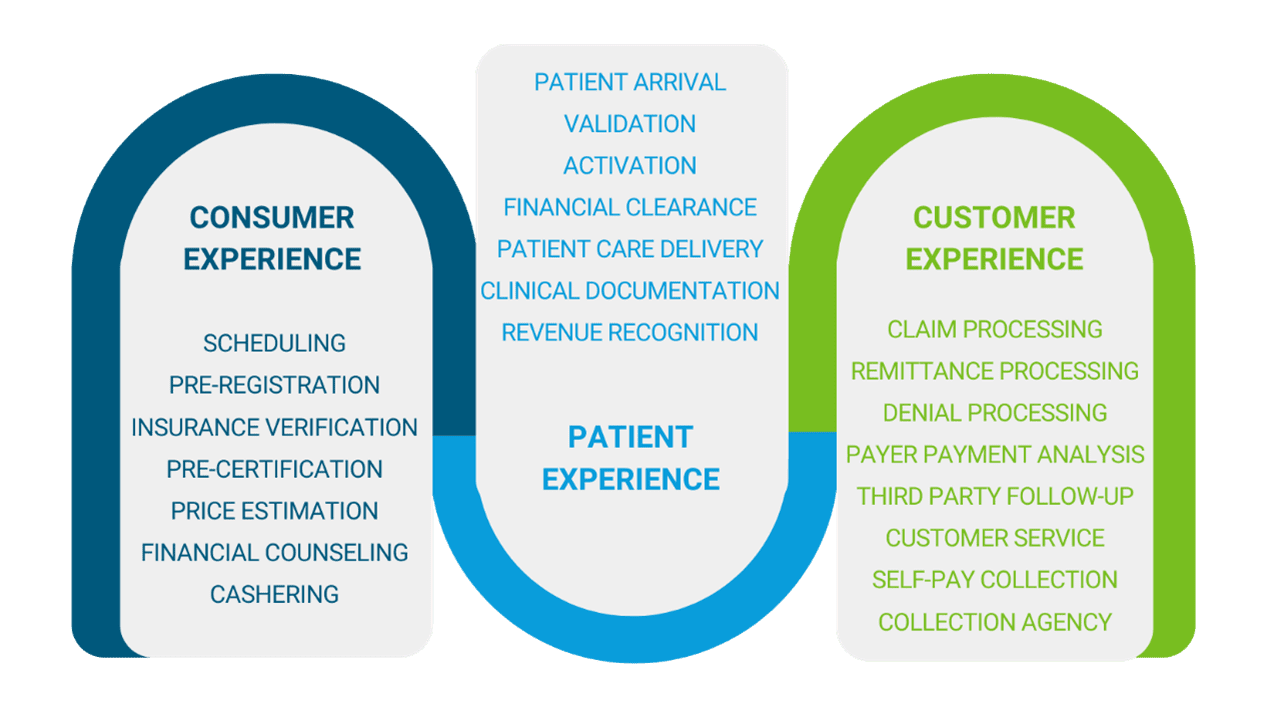
“The problem with this is that everything should be done accurately and efficiently prior to claim generation to get the claim out the door and paid on the first submission. Errors in front-end processes such as registration, patient demographics, insurance verification, and eligibility can cause all the things done right after that point to be thwarted and result in a denial. Every person that touches data that ends up on a claim or aids in the care and documentation process that supports billing and reimbursement, needs to understand they are part of revenue cycle and how they impact the organization’s KPIs,” said Scott.
Since the COVID-19 pandemic, the widespread adoption of remote work has caused revenue cycle managers to rely on data and dashboards to monitor productivity. They can no longer walk the floor, chat with team members, and keep tabs on the work everyone is doing. Fortunately, there are still effective ways to ensure your organization is meeting or exceeding benchmarks.
What are revenue cycle management KPIs?
KPIs are critical indicators of progress toward an intended result. They provide an evidence-based focus for operational and strategic improvements by showcasing success and efficiency or calling attention to areas of concern.
Selecting and monitoring KPIs is a proven way to optimize your revenue cycle management. Reviewing your revenue cycle KPIs frequently helps determine where your revenue cycle has opportunity for improvement, whether you should invest in education for your team, or — if KPIs are severely underperforming — you should seek revenue cycle management services.
Code and charge accuracy
The first set of recommended KPIs pertains to ensuring that medical coding accurately reflects patient conditions and properly documents the care they received. Coding accuracy also includes capturing information beyond DRG (Diagnosis Related Group) codes, such as physician and date of service information.
Compliance efforts encompass every aspect of the coding process to ensure accuracy and prevent fraudulent activity. KPIs to track to monitor include:
Medical coding accuracy: Coding specialists and teams should aim for an accuracy rate of 95% when coding individual records. Aim for even higher accuracy rates when coding DRGs. Low coding accuracy can lead to unfavorable audit results.
First pass resolution rate: This KPI measures the percentage of claims that get paid on first submission. Tracking this data will show the overall effectiveness of your revenue cycle and can reveal process alignment issues. Lower percentages can indicate that areas of your revenue cycle require corrective action.
Missed charges: Revenue cycle managers should investigate missed charges to detect patterns that could be preventing you from receiving reimbursement on a recurring basis. Errors can occur for a variety of reasons, including human error or technology issues. By catching problems early, organizations can avoid losing payments and maintain patient trust.
Code and charge productivity
Coding and charging managers should monitor coding and billing errors to ensure correct reimbursement. Additionally, they should make sure claims are filed as soon as possible to avoid delays in billing and payment.
Three KPIs that revenue integrity managers should monitor for code and charge productivity include the following:
Charge capture lag time: Tracking lag time can help identify delays in the charge capture workflow by revealing problems in getting patient information to the coding staff or completing documentation.
Discharged, not final billed (DNFB): Revenue managers can track the number and dollar amount of DNFB files to diagnose and solve workflow issues. A significant number of claims that await coding/billing could be a cause for concern. Find out why these items are pending, and work to reduce items with this status.
Coding productivity: Revenue cycle managers should aim for coding productivity of 95% or higher. This means no more than 5% of the coding load should be in queue at any given moment. However, the volume of coding will not decrease by simply adding more coders to the mix if the underlying problem is with process or technology.
Revenue reconciliation
Four KPIs can help you gather insights on revenue reconciliation: denial volume, denial appeal rate, days in receivables outstanding (DRO), and underpayment recoveries. By understanding how these numbers change over time, you can identify areas needing improvement and make changes to avoid revenue loss.
Denial volume: On average, claim denials cost healthcare organizations 5% of their net revenue. To avoid lost revenue, analysts look at denial percentages and the dollar amounts from denied claims. Denial rates typically range from 5% to 10%. By analyzing denial patterns, you can improve or automate workflows to ultimately achieve a higher claim approval rate.
Denial appeal rate: Tracking denial appeals allows revenue cycle managers to compare the total number of denials appealed to the total volume of denials. A high percentage of appeals is ideal. A low percentage of appeals may mean there are opportunities for automatic write-offs or adjustments.
Days in receivables outstanding (DRO): DRO tracks the average number of days it takes to collect payments. A high-performing billing department takes an average of 30 days or less to collect all payments due.
Underpayment recoveries: Becker’s Hospital CFO Report estimates that hospitals fail to collect 2% to 5% of net patient revenue. Revenue cycle managers should monitor underpayments and measure the success of efforts to recover those dollars.
To ensure that your organization is performing as expected, it’s important to monitor a range of metrics related to revenue integrity. These metrics can help identify areas where compliance risks are high and payment processing can be improved. By fixing these problems, you can improve your company’s overall performance.
Revenue cycle management and KPI support
Some of the benefits of having an optimized revenue cycle include increased cash flow, reduced cost to collect, greater point-of-service cash collections, and fewer denials. The revenue cycle must be efficient and effective from start to finish. Otherwise, you risk revenue leakage.
Executives face incredible challenges when it comes to managing the revenue cycle. The variables and contributing factors affecting your revenue cycle can become overwhelming. How do you know when it’s time to seek assistance?
Scott advised that it may be time to hire revenue cycle assistance if underperforming KPIs include bad debt, charity, cash-to-net revenue, credit balance in accounts receivable, billing turnaround, and a low percentage of claims paid on the first pass.
Relias offers a robust library of online courses that allow you to invest in your staff’s coding education, which can in turn impact your overall revenue cycle. If you’ve determined you need additional assistance, Revenue Cycle Coding Strategies offers expert revenue cycle analysis and optimization to help you improve your processes.
About our partnership with Revenue Cycle Coding Strategies
Relias partnered with Revenue Cycle Coding Strategies (RCCS) to offer resources to ensure that your coding is compliant and to help optimize your revenue cycle. In addition to quality online courses from Relias to invest in your staff’s coding education, RCCS offers a variety of outsourced solutions including coding audits, documentation reviews, coding professionals, and expert resources.
About Revenue Cycle Coding Strategies
Revenue Cycle Coding Strategies has provided specialty medical coding, revenue cycle, and compliance consulting services, as well as educational and training materials to the healthcare industry for over 20 years. RCCS has an extensive team of specialized coding experts and industry leaders who create and implement customized revenue cycle solutions, including billing auditing and assessments, compliance reviews, in-depth process mapping, and customized outsourced options.
How strong is your revenue cycle management process?
Two key components of a solid revenue cycle management process are timeliness and accuracy. With all the variables that come into play, it can be difficult to tell how efficient your organization is. How do you know if your revenue cycle and coding processes are optimal? Our guide can help provide insights to direct you in your analysis.
Access the guide →





