Value-based reimbursement is not new for healthcare. With more and more payments tied to performance and outcomes, Medicare is proposing that 90% of their reimbursements will be tied in some way to quality by the end of this year.
However, as a small, rural, or critical-access hospital, there are often different regulations or options for navigating a value-based world. Sometimes the best leverage these organizations have is that payers rely or these services for their members when access is limited to one facility for miles and miles. Utilizing this leverage, to maximize reimbursements, is the best way to secure your finances in the face of diminishing margins.
How Various Payers Participate in Value-Based Payment
Medicare, Medicaid, and commercial payers all have varying options and mandates for participation in value-based reimbursement. It is essential to understand the requirements associated with each payer to have a clearer picture as to where your organization can be the most competitive to maximize revenue across all funding streams.
Medicare
Since 1993, Medicare has reimbursed hospitals utilizing the Impatient Prospective Payment System. A prospective payment system uses predetermined rates for episodes of care. This could mean that there is one price for all single total knee replacements, regardless of length of stay, complications, resources utilized, etc. Medicare categorizes patients according to their Medicare-severity adjusted Diagnosis Related Group (MS-DRG). These categorizations consider a patient’s diagnosis and severity of illness to determine the rate for that admission. It is important to note that critical-access hospitals (CAHs) are exempt from IPPS participation; however non-CAH, small or rural hospitals would still receive Medicare payments through this system.
Additional payment models for Medicare include:
- The Readmission Program – reduces payment for excessive readmissions for the following diagnoses: acute myocardial infarction, heart failure, pneumonia, chronic obstructive pulmonary disease, total hip/knee arthroplasty, and coronary artery bypass grafting.
- The Hospital Acquired Condition Reduction Program – decreases payment by one percent for the lower performing 25% of hospitals regarding their number of hospital-acquired conditions.
- Value-Based Purchasing Program – reduced all DRG payments by two percent to create an incentive pool, allowing hospitals to earn back less than, some/all, or more than the reduction in relation to how they perform on specific quality measures.
Medicaid
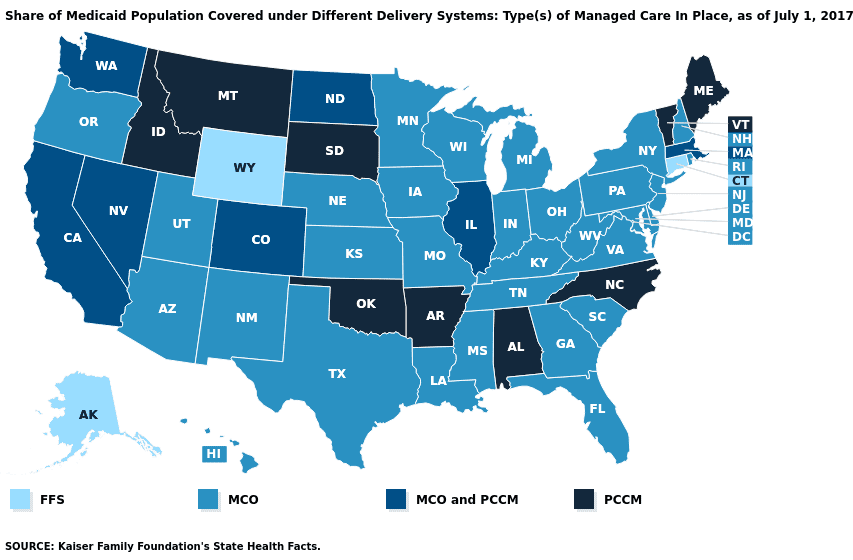
Many states have optional or required participation in Medicaid managed care. State Medicaid programs will partner with Managed Care Organizations (MCOs) to provide capitated payment to all their members. Capitated payment is like prospective payment, except instead of rates being for an admission or episode of care, the MCO and state will have an amount of money per member that can be utilized for all their monthly or annual expenses.
Across the United States, nearly 75% of Medicaid patients receive care through managed care programs. These programs include:
- Comprehensive-risk based managed care – covers inpatient hospital services and a combination of additional outpatient services.
- Primary Care Case Management (PCCM) – payment to primary care provider for care management and coordination, while provider is still paid using a fee-for-service model.
- Limited-benefit plans – a specific set of specialized services are paid through the plan.
Commercial Payers
Commercials payers are also participating in value-based reimbursement. However, the programs will vary across each specific payer. There are some more typical arrangements, including:
- Accountable Care Organizations (ACOs) – Groups of providers and healthcare facilities/organizations that come together to provide coordinated care to their patients/members, sharing financial risk and savings.
- Bundled payments – Set reimbursements for certain episodes of care with total knee/hip being common with commercial payers.
- Risk-based contracting – Reimbursement contracts that place some risk on the provider/organization, ranging from bundled payments to full capitation.
The 5 Keys to Success
Given all the options for value-based participation across the varying payers and funding streams, there are five steps to ensure success and maximize reimbursements for small and rural hospitals.
1. Understand the value-based reimbursement options or mandates across your payments.
The above list is not exhaustive. Depending on your individual payers and states where you provide services, the options could be endless for value-based participation. It is important to understand what is required and what additional options exist before moving forward.
2. Analyze where your organization performs well above benchmarks.
It is quintessential for your organization to be data-driven. Whether you utilize your EHR or have a home-grown or vendor-purchased analytics engine, knowing how you are performing in specific measures and with specific diagnoses will be invaluable to choosing how you will participate. Focus first on where you are currently performing well above benchmarks and can immediately capture some additional payment.
3. Analyze areas of weaker performance that are low-hanging fruit.
Next consider where you are not yet performing in the top percentiles but could easily incorporate process changes or education to improve your performance. These areas will be next on the list when choosing which programs and which measures or patient populations where you will want more money tied to quality.
4. Prioritize areas that maximize reimbursement across payers.
Now that you have your analyzed data and target areas, consider where multiple payers have programs that address these metrics. You will then narrow your plans even further to areas that will be easy for you to maintain or achieve top performance and will garner increased reimbursement from multiple funding streams.
5. Utilize leverage to create risk-based contracting that favors your organization.
As an organization that provides services to patients/members who have limited access to healthcare organizations, you are a necessary provider for any payers servicing members in that area. Use this leverage to negotiate risk-based contracts, especially with MCOs or commercial payers, that include your target areas.
Summary
Small and rural hospitals have many options for value-based payment participation. Make sure you are leveraging the critical services you provide to structure payment contracts in your favor. Also, consider where you are going to get your data and what interventions you will use to continue in high performing areas and to improve in others to ensure success and maximize reimbursements.
Learn more about how Relias is committed to helping rural and critical access hospitals with affordable solutions through our partnership with the National Rural Health Association (NRHA).






