Near the end of July, SNF providers will have their SNF Five-Star ratings updated. SNF providers will notice several differences in how the star ratings are calculated and these differences may have an impact on your facility’s overall Five-Star rating. In this article we will highlight the major differences announced by CMS.
SNF providers can get more in-depth information by reviewing the newly released SNF Five-Star Quality Rating System Technical User’s Manual, July 2016.
Quality Measures used in the Five-Star Quality Reporting System
The most noticeable difference providers will see is the change in the total number of QMs used in the SNF Five-Star rating system. The number of quality measures utilized for the July 2016 quarterly update has increased from 11 to 16. Earlier this year, CMS implemented 6 new quality measures. Of these six, five are being used in the quality measure component of the Five-Star rating system, including the three new claims based measures.
The 16 quality measures used in the Five-Star system are:
Short Stay measures:
- Percentage of residents with pressure ulcers that are new or worsened
- Percentage of residents who self-report moderate to severe pain
- Percentage of residents who newly received an antipsychotic medication
- Percentage of residents whose physical function improves from admission to discharge (NEW)
- Percentage of residents who were re-hospitalized after a nursing home admission (NEW claims based measure)
- Percentage of residents who have had an outpatient emergency department visit (NEW claims based measure)
- Percentage of residents who were successfully discharged to the community (NEW claims based measure)
Long Stay measures:
- Percentage of residents whose need for help with activities of daily living has increased
- Percentage of residents whose ability to move independently worsened (NEW)
- Percentage of high risk residents with pressure ulcers (long-stay)
- Percentage of residents who have/had a catheter inserted and left in their bladder
- Percentage of residents who were physically restrained
- Percentage of residents with a urinary tract infection
- Percentage of residents who self-report moderate to severe pain
- Percentage of residents experiencing one or more falls with major injury
- Percentage of residents who received an antipsychotic medication.
Quality Measure Summary Scoring System
Due to the addition of the five new quality measures, the current scoring system used to determine each facility’s QM summary score and subsequent Five-Star rating has also changed. It should be noted, for the first two quarters (July and October), the five new measures will be phased in and only be assigned one-half (505) of the points compared to the other 11 measures.
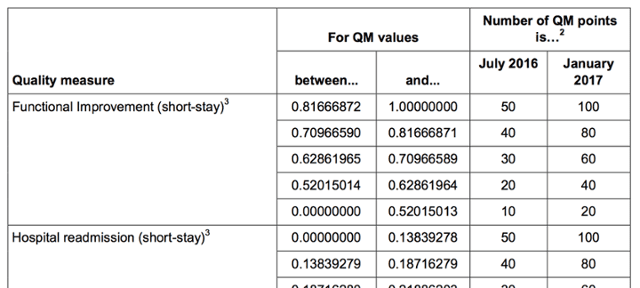
For each of the QMs, 20 – 100 points are assigned based on the facility’s performance in that particular QM. For the five new QMs, points will range from 10 – 50 points (50%) during the 6-month phase in period. Once the points are assigned for each QM, the sum of these points will determine the facility’s QM Five-Star rating.
To assist providers in analyzing their QM scores, CMS has updated the QM Point Value tables in the July 2016 SNF Five Star Rating System Technical User’s Manual.
The SNF provider’s QM summary score can now range from 275 – 1350 points. The breakdown in point ranges is shown in the following table:
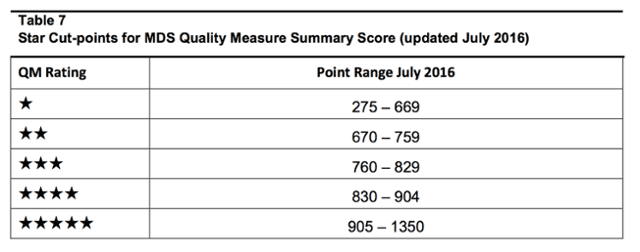
The QM summary score range will be updated again in January 2017, when the phase in period for the five new QMs is completed, and all quality measures will be assigned 20 -100 points. The new QM summary score range, effective in January 2017, will be 325 – 1,600 points.
Other Five Star QM Computation Changes
- Increase from Three Quarters to Four Quarters – beginning with the July 2016 update, CMS will begin using the most recent four quarters of available data where previously CMS had only used the most recent three available quarters. CMS reports that the increase in quarters will increase the stability of estimates and reduces the amount of missing data.
- Minimum denominator changed – CMS has standardized the minimum number of assessments required in order to calculate the MDS-based measures. For both short and long-stay QMs at least 20 MDS assessments, across the four quarters, must be available. For claims-based measures, at least 20 nursing home stays must have occurred over the course of the year.
- Missing data or denominator not met – CMS has also made changes to the calculation of QMs for those facilities that have missing data or inadequate denominator size (20 MDS assessments). For further details, refer to the Five-Star Rating System Technical User’s Manual, July 2016.
- Changes to ADL QM Calculation – in the past, CMS used state-specific cut-point thresholds for assigning points for the ADL QM. With the July 2016 update CMS has changed to using national cut-points.
- Changes to Reports – CMS also indicates that the facility’s Five-Star reports will now also include the assigned number of points for each of the quality measures. This will assist providers in their analysis and understanding of their QM Five-Star rating.
It is important to note that no changes have been implemented to the Health Inspection or Staffing components of the Five-Star rating system. In addition, the overall Five-Star rating will be determined using the same process used in previous years, as outlined here.
Step 1: Start with the health inspection rating.
Step 2: Add one star to the Step 1 result if the staffing rating is four or five stars and greater than the health inspection rating; subtract one star if the staffing rating is one star. The overall rating cannot be more than five stars or less than one star.
Step 3: Add one star to the Step 2 result if the quality measure rating is five stars; subtract one star if the quality measure rating is one star. The overall rating cannot be more than five stars or less than one star.
Note: If the health inspection rating is one star, then the overall rating cannot be upgraded by more than one star based on the staffing and quality measure ratings. If the nursing home is a Special Focus Facility (SFF) that has not graduated, the maximum overall rating is three stars.
Providers should take great care in reviewing their new Five-Star reports and determining the impact that these changes may have had on their overall Five-Star rating and take appropriate steps, if applicable, to improve their QM ratings.






