A New Mother’s Experience with Sepsis
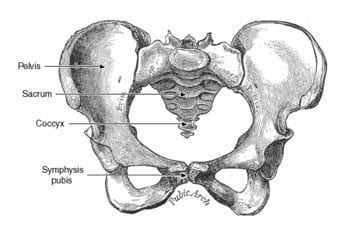
A 34-year-old woman left the hospital after delivering her first baby. A complication of the delivery included a four-cm separation of the symphysis pubis, which required that she go home with pain medications and follow up with physical therapy. This wasn’t the start she had imagined, but she headed home with a healthy baby in tow, and that was enough.
 Two short days later she began to experience chills and shakes accompanied by a fever of 100 degrees. She called into the OB and was told the symptoms were likely due to her breast milk coming in. The OB recommended that she try to rest more between feedings. That night she woke with shakes in a cold sweat, a fever that had risen to 104 degrees, a heart rate in the 120s, a respiration rate of 25, and severe lethargy.
Two short days later she began to experience chills and shakes accompanied by a fever of 100 degrees. She called into the OB and was told the symptoms were likely due to her breast milk coming in. The OB recommended that she try to rest more between feedings. That night she woke with shakes in a cold sweat, a fever that had risen to 104 degrees, a heart rate in the 120s, a respiration rate of 25, and severe lethargy.
Something was wrong. An ambulance was called.
This new mother was rolled out of her home in a stretcher to the ambulance. Sensing an impending doom, she said her tearful goodbyes to her husband and newborn child. Thankfully, the woman in this story recovered, but had she thought this was all part of the “new normal” post childbirth. Her story may have been very different.
Three hours – about the same time it would take you to watch the Titanic or a musical at the theater.
Three hours – the short window of time to identify sepsis.
Sepsis Identification and Treatment in the U.K.
While many ICU, CCU and ED doctors are now more aware of and able to recognize the presentation of sepsis, will front-line staff in other disciplines be prepared to identify sepsis? While some patients may go straight to the emergency department, others may find their first line of medical contact to be their family physician or the doctor attending to their most recent medical need.
In the U.K., through Project Transform, a decision-making training was introduced with the learner taking the role of a General Practitioner, Emergency Room doctor, or healthcare assistant. While not developed specifically for the US, this resource does a wonderful job of pointing out the time sensitivity when identifying and treating sepsis.
The U.K. has also moved towards a national scoring system for identifying sepsis early known as the National Early Warning Signs (2). This tool has been critical in the hand-offs of care between front-line physicians, Emergency Medical Technicians, and the arriving hospital as outlined by providers of care in this video. Through the implementation of uniform tools, the patient’s progression or deterioration can be monitored by universal standards and appropriately prioritized.
Surviving Sepsis Campaign in the U.S.
In the U.S., Apache II scores are used as predictors of mortality in ICU and CCU units, but are not necessarily intended as a tool to identify sepsis. However, the Surviving Sepsis Campaign in the US launched an App that provides screening tools to assist in identifying patients with sepsis and allows users to set up bundle alerts.
As mentioned in Today’s Hospitalist, “The Surviving Sepsis guidelines are a matter of intervening quickly. In trauma, you have the golden hour; in stroke, you have the window to treat with thrombolytics; and in acute MI, ‘time is muscle.’ When it comes to sepsis, it’s almost the same kind of principle.”
While there is not a universal screening tool across the U.S., through the work of the Surviving Sepsis Campaigns, bundles by hour blocks are outlined for a clear clinical path when sepsis is suspected.
Leaders of the Society of Critical Care Medicine and the American College of Emergency Physicians have expressed concerns about the recently released SSC 1-Hour Bundle and have recommended that hospitals in the US refrain from implementing the bundle in its present form.
In contrast, the Sepsis 3-Hour bundle remains a commonly used standard across US hospitals. Findings released in fall of 2018 indicate that roughly half of U.S. hospitals do not follow the CMS recommended sepsis shock treatment guidelines. Yet, doctors are still optimistic about moving towards standardization of measurement and clarity of medically necessary protocols for all sepsis patients.
Final Thoughts
If your organization is among the many working to determine the best clinical and operational pathway for the identification, treatment, and management of sepsis patients, you are not alone. Several hospitals have made their tools and resources available for others.
Improve Quality of Care With Reliable Teams
Learn more about how to provide high-quality education to build the best patient care teams.
Learn More →





