Recruiting and Staffing
Recruit best-fit nurse talent and reduce turnover with our proprietary talent matching and validated assessments to find the right nurse with the right skills at the right time.
Learn more
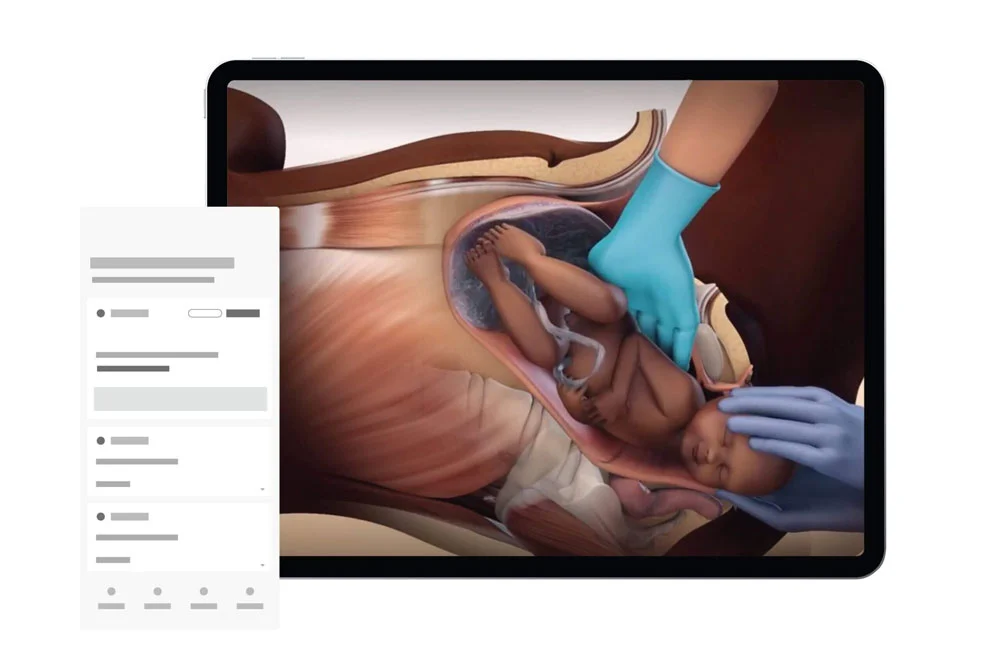
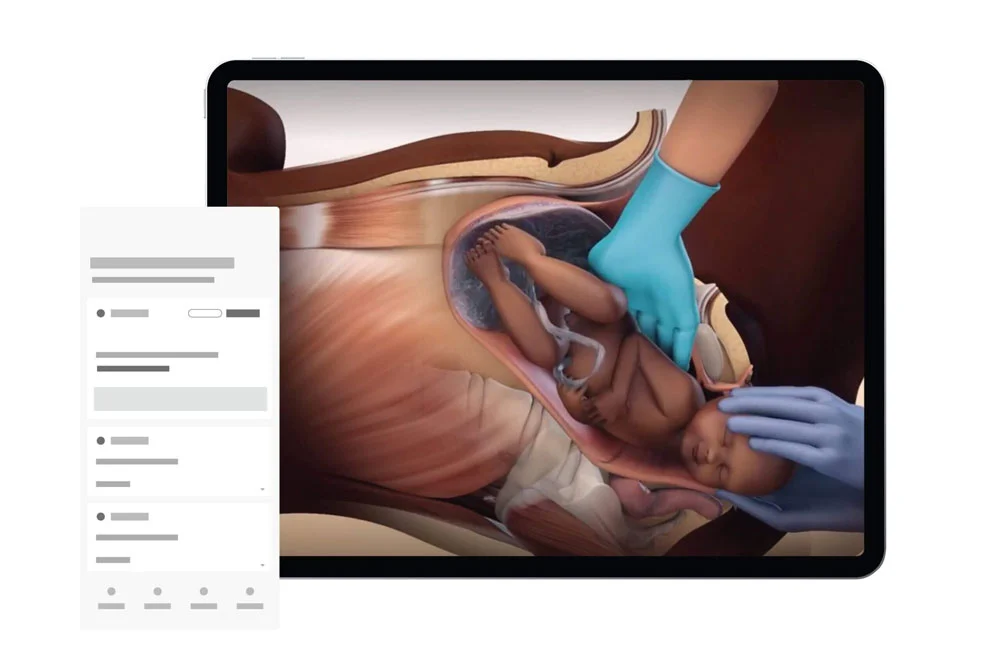
Learning and Performance
Educate and develop your staff with accredited, award-winning content and competency solutions that ease the administrative burden, support your compliance, and keep your staff engaged.
Learn more
Compliance Management
Reduce risk and build a culture of compliance with easy-to-maintain training and compliance solutions that keep pace with regulatory change and help organizations avoid penalties.
Learn more
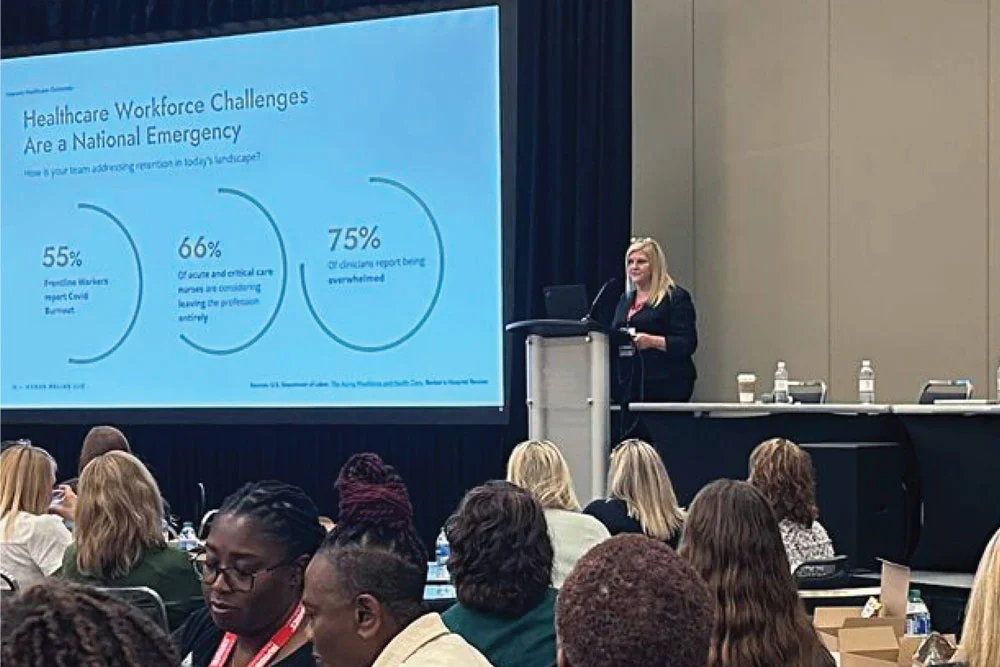
Why Relias
Knowledge is at the core of who we are and what we do. Relias has over 3,000 courses built by in-house healthcare and adult learning experts. Our education solutions ensure that your workforce has access to the knowledge it needs to provide the best care.
Learn More
The technology behind Relias better engages your staff and focuses on simplifying your responsibilities and improving the care you provide. The Relias Platform, content delivery tools, and integration capabilities save you time, promote course completion, and create compliance.
Learn More
We understand that your time and resources are limited. Relias’ customer success, support, and professional services teams are here to provide end-to-end support to customize, implement, and integrate our solutions into your existing platforms and systems. We’re your partner every step of the way.
Learn More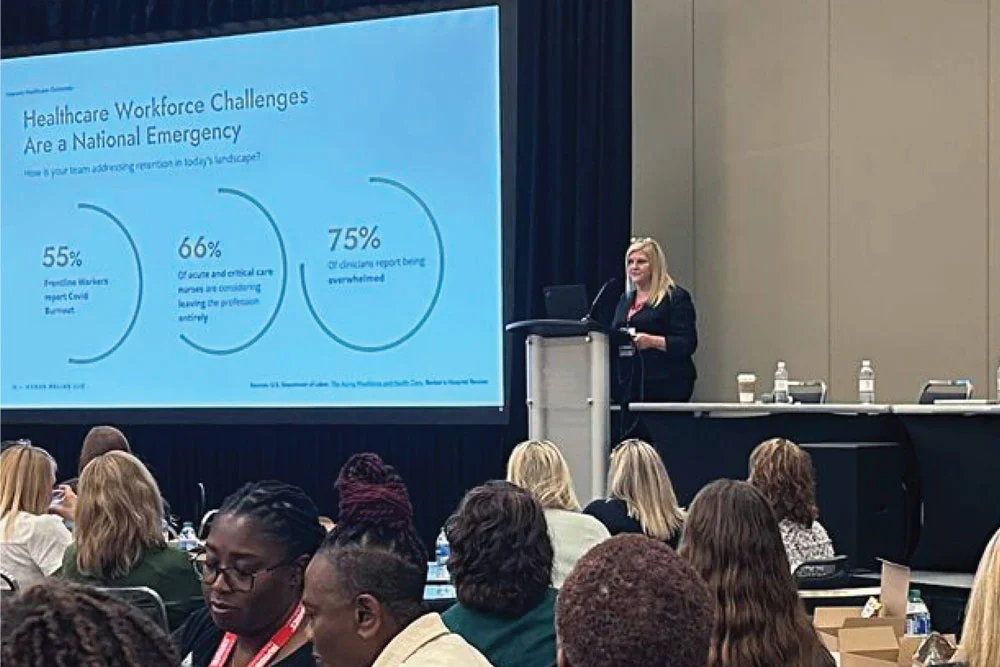
We understand you because we are you. Our in-house clinicians work every day to ensure that our best-in-class education, expert guidance, and industry insights will move your organization and your workforce forward.
Learn More
We believe a strong community of healthcare workers yields better outcomes for everyone. Our online communities connect nurses, physicians, allied health professionals, and learning administrators and reinforce the value of learning for all healthcare workers to give them the resources and support they need to thrive.
Learn More