During the SNF Open Door Forum (ODF) held on Thursday, March 3 CMS introduced six new Quality Measures that will be reported on the Nursing Home Compare (NHC) website in April 2016. The six new Quality Measures that will be reported on NHC will include four short-stay measures and two long-stay measures. In addition, three of the new Quality Measures will be claims-based measures. This is a significant departure from the usual MDS-based Quality Measures, of which the SNF industry is accustom.The claims based short-stay measures will be calculated for Medicare Part A residents only. The QMs will not include Medicare Advantage plan residents.
The Six New Measures
Short Stay
- Percentage of short-stay residents who were successfully discharged to the community (claims based).
What it measures: To Identify residents who were successfully discharged to the community within 100 days of admission to the SNF and who are not admitted to a hospital (inpatient or observation), a nursing home, or expire within 30 days of discharge.
- Percentage of short-stay residents who have had an outpatient emergency department visit (Claims-based).
What it measures: Identifies residents seen in a hospital emergency department within 30 days of admission to the SNF that did not result in an inpatient or observation stay. Resident must have been admitted to the SNF following an inpatient hospital admission.
- Percentage of short stay residents who were re-hospitalized after a nursing home admission (Claims-based).
What it measures: Identifies residents readmitted to the hospital as an inpatient or under observation stays within 30 days of admission to the SNF. Includes residents that may have been discharged from the SNF but still within the 30-day period. Planned readmissions will be excluded.
Based on the information provided thus far, this readmission QM does appear to have some significant differences from the readmission QM approved for use in the SNF Value Based Purchasing (VBP) program.
- Percentage of short-stay residents who made improvement in function (MDS based).
What it measures: Identifies residents who demonstrate an improvement in the following three ADLs: transfer, locomotion on unit, and walk in corridor. A comparison will be made between the 5-day SNF PPS assessment and the Discharge Return Not Anticipated assessment. Will exclude hospice residents or those residents with a life expectancy of 6 months or less.
Long Stay
- Percentage of long-stay residents whose ability to move independently worsened (MDS-based).
What it measures: Identifies residents who experience a decline in their ability to move around in their room and in the adjacent corridor. This will be determined by comparing the most recent assessment to the prior assessment. Certain exclusions and risk adjustments will be applied.
- Percentage of long-stay residents who received an antianxiety or hypnotic medication (MDS-based).
What it measures: Identifies long-stay residents who receive any number of antianxiety or hypnotic medications. Will exclude residents on hospice or with a life expectancy of less than 6 months at the time of the assessment.
It should be noted that the anti-anxiety/hypnotic medication use QM would not be the same as the current anti-anxiety/hypnotic medication QM that includes specific exclusions based on resident diagnoses. At the time of the ODF, CMS has not yet released the QM Technical Specs that would provide the in-depth level of detail required to understand how each of these quality measures will be calculated. CMS has however developed a summary of the new QMs as part of their SNF ODF presentation and is available for viewing here: CMS also indicated that while NHC will report each of these new QMs they would not be immediately available on facility CASPER reports. CMS has plans to update those reports at a later date. CMS has indicated, however, that they will issue preview reports for each facility approximately the third week of April that can be accessed via the QIES system.
Impact on Nursing Home Five-Star Rating Program
In addition to posting these new QMs on the Nursing Home compare website, CMS will also be incorporating five of these six quality measures into the nursing facility Five-Star rating system beginning in July 2016. The QM for long-stay residents receiving an antianxiety or hypnotic medication is the only QM of the six that will not be used in the calculation of each nursing facility’s Five-Star rating. The Five-Star rating system is comprised of three different components: Health Inspections, Staffing and Quality Measures. The five new Quality Measures will be factored into the QM component of the overall nursing facility Five-Star rating. Currently the QM Five-Star component for each facility is based on the following QM Summary Score cut points: 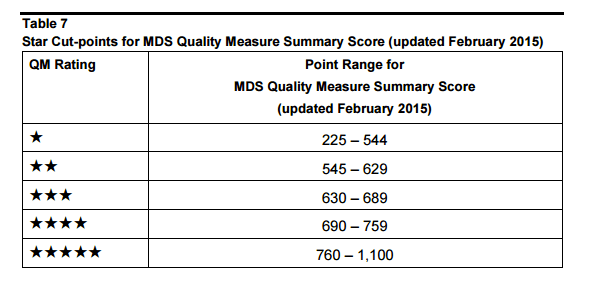 CMS has yet to release any specific information on how the five new measures will impact the overall QM Five-Star scoring. CMS did however state, that they will implement a nine-month phase-in process of these new QMs into the Five-Star program. CMS anticipates an updated Five-Star Quality Rating System Technical User’s Manual will be available prior to the July implementation of the new Five-Star rating. It is anticipated that some facility’s Five-Star QM ratings may change based on the introduction of these new QMs but without the specifics it is difficult to ascertain the degree of change that may occur or how that change may impact the facility’s overall Five-Star rating
CMS has yet to release any specific information on how the five new measures will impact the overall QM Five-Star scoring. CMS did however state, that they will implement a nine-month phase-in process of these new QMs into the Five-Star program. CMS anticipates an updated Five-Star Quality Rating System Technical User’s Manual will be available prior to the July implementation of the new Five-Star rating. It is anticipated that some facility’s Five-Star QM ratings may change based on the introduction of these new QMs but without the specifics it is difficult to ascertain the degree of change that may occur or how that change may impact the facility’s overall Five-Star rating






