October 1 is fast approaching which means that SNF providers need to be aware of and up to speed on changes to the MDS process and coding directives. As a follow up to our recent webinars on the various changes we are providing you with a summary of what is in store come October.
Implementation of Section GG
CMS will be implementing the new Section GG – Functional Abilities and Goals. This new section will be required to be completed on all Medicare 5-day PPS assessments and SNF Part A PPS Discharge assessments effective 10/1/2016.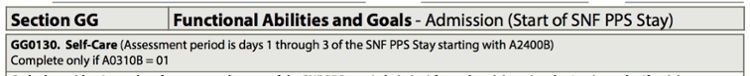
Section GG is being implemented in order to meet the statutory requirements of the IMPACT Act’s Function Quality Measure being implements as part of the SNF Quality Reporting Program (SNF QRP).
The purpose of this section is to be able to accurately assess a resident’s functional abilities upon admission (baseline) as well as upon discharge from their Medicare Part A SNF say.
In addition, at least one discharge goal will need to be established and identified on the 5-day assessment for any of the functional areas in GG0130 or GG0170. Providers may include more than one discharge goal if they so desire.
New SNF PPS Part A PPS Discharge Assessment
The new SNF Part A PPS Discharge assessment is also being implemented as of 10/1/2016. This new discharge assessment will be required to be completed on residents who end a Medicare Part A stay and remain in the facility.
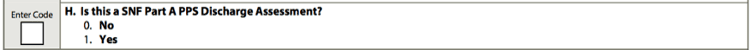
This new discharge assessment will consist of clinical data elements from MDS 3.0 Sections GG, J and M. This data will be utilized to calculate the three quality measures utilized in the upcoming SNF QRP: Functional status, Pressure Ulcers and Falls with Major Injury.
The SNF Part A PPS discharge assessment will be required in addition to the OBRA Discharge assessments currently being completed when a resident ends their Medicare Part A stay and is subsequently physically discharge from the facility. CMS will allow these two types of discharge assessments to be combined if the actual date of discharge is within one day of the end date of their Medicare stay. The SNF Part A PPS Discharge assessment will not be required if a resident expires or is unexpectedly discharged (unplanned).
Example 1: Medicare A stay ends/Remains in the SNF.
Discharge Requirements: SNF Part A PPS Discharge assessment only.
Example 2: Medicare Part A stay ends on 10/10, resident is discharged to home on 10/11.
Discharge Requirements: OBRA Discharge assessment and SNF Part A PPS Discharge assessment which may be combined.
Example 3: Resident is unexpectedly discharged to the hospital and admitted.
Discharge Requirements: OBRA Discharge assessment only.
Clarification and Revision to “Present on Admission” Rules (Section M)
CMS made a couple of coding changes related to how we determine if a pressure ulcer is to be coded as “Present on Admission”. The following coding revision better defines those pressure ulcers that are not facility acquired as present on admission and those that are facility acquired as not present on admission.
If a resident who has a pressure ulcer that was “present on admission” (not acquired in the facility) is hospitalized and returns with that pressure ulcer at the same numerical stage, the pressure ulcer is still coded as “present on admission” because it was originally acquired outside the facility and has not changed in stage.
This change in coding guidance coincides with the recent calculation change in the Pressure Ulcer SNF QRP QM that will now utilize the “Present on Admission” items on the MDS to determine if a pressure ulcer is a new or worsened pressure ulcer.
SNF Staff responsible for coding Section M will want to review all rules related to coding “present on admission” to ensure it is coded accurately.
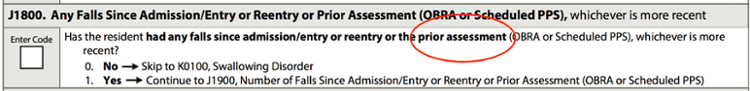
Clarification related to which assessments qualify as “Prior Assessments”
The RAI manual update contained a clarification related to which assessments should be utilized when an MDS 3.0 question is referring to a “prior assessment”. SNF providers should only be using those assessments that are submitted to the QIES ASAP system. Assessments completed for private insurance and Medicare Advantage plans are NOT to be submitted and should not be considered when determining the “prior assessment”.
Coding of Injurious Falls Goes Beyond the ARD (Section J)
Since Falls with Major Injury is currently a quality measure and will also be a measure utilized in the SNF QRP, CMS wants to ensure that this item is coded accurately. The purpose of this MDS 3.0 item is to determine if any falls resulted in no injury, injury (minor) or a major injury.
To accurately determine the level of injury CMS has clarified that SNF providers should use all available documentation available in making this determination, even if that documentation is received after the assessment reference date (ARD) of the assessment.
If the level of injury directly related to a fall that occurred during the look-back period is identified after the ARD and is at a different injury level than what was originally coded on an assessment that was submitted to QIES ASAP, the assessment must be modified to update the level of injury that occurred with that fall.
All staff members involved in the completion of the MDS should review the final <DS 3.0 RAI User’s Manual updates and revisions for more specifics related to the items discussed above as well as a few other minor revisions. The RAI Manual can be found on the CMS website here.






